vtach
- related: tachycardia
- tags: #note
EKG characteristics
In adult patients with structural heart disease, 95% of wide-complex tachycardias are VT. Several important clinical and ECG features can distinguish VT from other conditions. Wide-complex tachycardias that are positive in lead aVR, have a QRS morphology that is concordant in the precordial leads, have QRS morphology other than typical right or left bundle branch block, and exhibit extreme axis deviation (“northwest” axis) are usually VT. AV dissociation, fusion beats, and capture beats are all highly suggestive of VT. When the origin of a wide-complex tachycardia cannot be determined, VT should be assumed until expert consultation can be obtained.
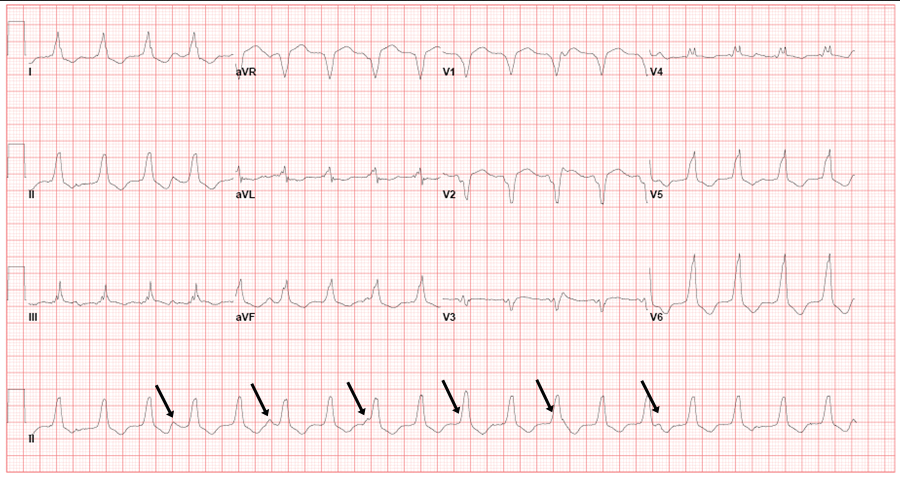 Electrocardiogram demonstrating a regular monomorphic wide-complex tachycardia in a left bundle branch block pattern. The presence of atrioventricular dissociation confirms the diagnosis of ventricular tachycardia. The arrows identify nonconducting P waves.
Electrocardiogram demonstrating a regular monomorphic wide-complex tachycardia in a left bundle branch block pattern. The presence of atrioventricular dissociation confirms the diagnosis of ventricular tachycardia. The arrows identify nonconducting P waves.
Structural Heart Disease
In ischemic and nonischemic cardiomyopathy, the presence of myocardial scar tissue facilitates a reentry circuit and the development of VT. VT is usually regular and monomorphic in patients with ventricular scarring. Sustained VT (≥30 seconds) can lead to hypotension, syncope, VF, and cardiac arrest; however, short episodes of VT (nonsustained) or slow sustained VT may be well tolerated or cause no symptoms.
Evaluation with resting ECG, exercise treadmill testing (to provoke arrhythmias), and cardiac imaging (to identify structural heart disease) is indicated in all patients with VT. Patients with ischemic cardiomyopathy who present with VT should be considered for angiography and revascularization if appropriate. Cardiac magnetic resonance imaging clarifies the extent and pattern of myocardial scarring, which can be helpful in refining the cause of the cardiomyopathy and can assist in determining prognosis. For example, patients with a higher burden of myocardial scarring have higher risk for recurrent arrhythmia.
β-Blockers and ACE inhibitors reduce the risk for sudden cardiac death (SCD) in patients with prior myocardial infarction and cardiomyopathy. In those with recurrent VT despite β-blocker therapy, antiarrhythmic drug therapy with amiodarone may be considered. Catheter ablation should be considered in patients with recurrent VT despite medical therapy. ICD placement is indicated for secondary prevention of SCD in patients with structural heart disease or cardiomyopathy who have sustained VT/VF, provided that reversible causes have been excluded (such as acute coronary ischemia or cocaine ingestion).
Idiopathic Ventricular Tachycardia
Idiopathic VT (so-called normal heart VT) occurs in the absence of structural heart disease, typically arising from the outflow tracts, fascicles, and papillary muscles. Patients with idiopathic VT usually present with palpitations in the third to fifth decades of life. Episodes of syncope are uncommon. Arrhythmic events are often triggered by stress, emotion, or exercise. These tachycardias are responsive to adenosine.
Calcium channel blockers, especially verapamil, and β-blockers are first-line treatment for idiopathic VT. Catheter ablation can be considered if symptoms continue despite these therapies. ICDs are contraindicated in patients with hemodynamically stable idiopathic VT, owing to the benign prognosis and efficacy of other therapies.