volvulus
- related: GI
- tags: #GI

Volvulus is due to an intestinal segmental torsion that may lead to obstruction or gangrene if untreated. It occurs most commonly in the sigmoid and cecum and less commonly in other portions of the gastrointestinal tract (eg, stomach, transverse colon, splenic flexure). Sigmoid volvulus is more common in elderly patients who are institutionalized or affected by neurologic or psychiatric conditions (eg, schizophrenia, Parkinson disease).
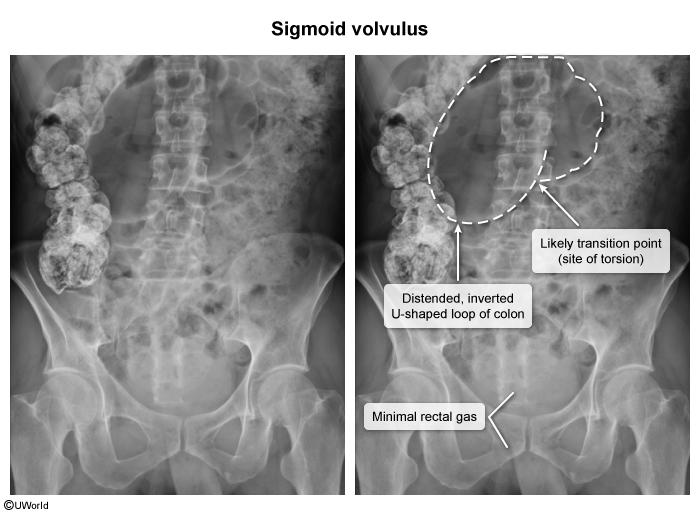
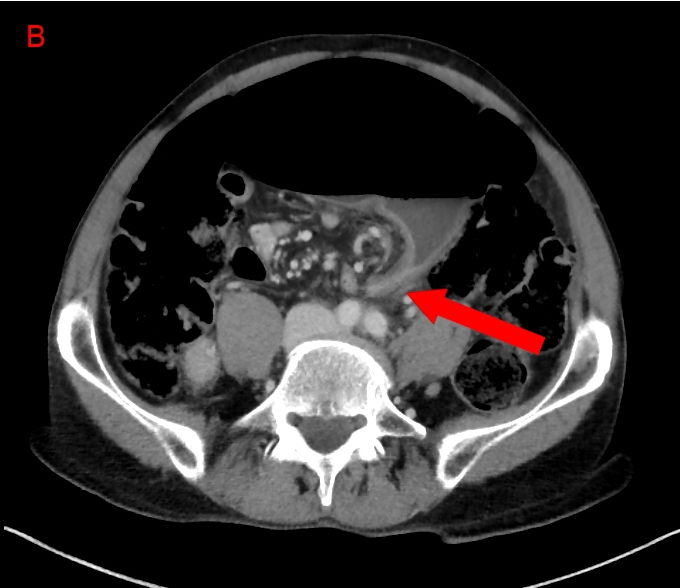
Patients typically complain of abdominal pain, distention, constipation, and nausea. Plain abdominal x-ray is diagnostic in 60% of cases. X-ray shows a large air-filled sigmoid colon that extends from the pelvis to the right upper quadrant and absence of air in the rectum. In addition, distended proximal large bowel and air-fluid levels in the small intestine are commonly present. Air under the diaphragm or outside the bowel wall usually indicates perforation. Computed tomography scan usually shows dilated sigmoid colon (whirl pattern) around the mesocolon and vessels creating a bird beak appearance. Barium enema with water-soluble contrast can be helpful when the diagnosis is uncertain.
Management is focused on preventing gangrene and correcting the underlying anatomic abnormality to reduce the risk of recurrence. Patients without gangrene or perforation (eg, fever, sepsis, peritonitis) need sigmoidoscopy to untwist the volvulus, restore blood supply, and assess colonic viability. However, sigmoidoscopy should be stopped if gangrene is present. Most endoscopists leave a rectal tube beyond the volvulus segment to further decompress the bowel and prevent recurrence. However, volvulus may reoccur in up to 60% of cases within a matter of hours to weeks. Surgery is reserved for patients with initial perforation/gangrene or recurrent volvulus despite conservative therapy.
Nasogastric suction is usually performed for complete or high-grade small-bowel obstruction to decompress the bowel. Antibiotics are not routinely administered for uncomplicated small-bowel obstruction.