upper GI bleed
Sx
- hematemesis: bright red blood/clots
- “coffee-ground” emesis: dark, digested blood
- melena: black, tarry stool
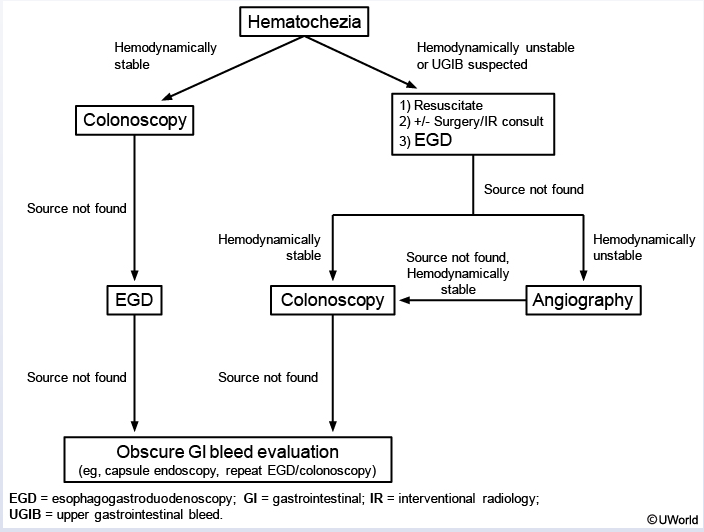
- hematochezia: bright bloody stool
Causes
- peptic ulcer disease: most commin, mostly by NSAID or H pylori
- esophagitis: rarely causes significant UGIB
- gastroesophageal varices
- usually in proximal stomach or distal esophagus
- Mallory-Weiss tear: from repeated vomiting/retching
- Less commonly
- Cameron erosions: Cameron lesions are erosions found on the crest of gastric folds within a large hiatal hernia and are thought to be caused by mechanical trauma as the hiatal hernia slides up and down. Up to 5% of patients with known hiatal hernias may have Cameron lesions.
- Dieulafoy lesion: submucosal arterioles that intermittently protrude through the mucosa and cause hemorrhage. Dieulafoy lesions are of unknown etiology and account for about 2% of all causes of acute upper gastrointestinal bleeding and are located in the proximal stomach along the lesser curvature. When bleeding they appear as an isolated pumping arteriole in the absence of a mass or ulcer.
- gastric antral vascular ectasia (GAVE)
- hemobilia
- tumors
- aortoenteric fistula
- hemosuccus pancreaticus
Management
- Intubation: AMS, massive bleed, risk of aspiration
- goal transfusion: 7 for stable and above for unstable
- over transfusion can increase variceal bleed due to increased portal pressure
- resuscitation with LR or NS is ok
- IV PPI
- octreotide, abx, BB: if variceal hemorrhage suspected
- continue octreotide 3-5 days
- IV erythromycin: improves gastric visualization. Only when requested by GI
- patients are at high risk for pneumonia/UTI. Use rocephin/quinolone for prophylaxis
- start abx for all patients with cirrhosis and GI bleed
- Continue abx for 7 days after bleed
- Start nonselective BB (propranolol, nadolol, coreg) for secondary ppx of variceal bleed. Increase BB to resting HR 55-60.
- Warfarin and supratherapeutic INR: vitamin K and PCC
- Discontinue secondary ppx ASA for 3 days but need to be resumed
- for NSAIDS: discontinue permanently
- if need for pain, use selective Cox-2 inhibitor celecoxib with PPI
- The modified Glasgow-Blatchford bleeding score
- blood urea nitrogen level
- hemoglobin level
- systolic blood pressure
- pulse rate
- It predicts the need for clinical intervention, rebleeding, and mortality. Patients at low risk with a modified Glasgow-Blatchford score of 1 or less may be considered for early discharge or outpatient treatment.
- Endoscopy should be performed within 24 hours of resuscitation
- in those with rapid bleeding or suspected variceal hemorrhage, it should be done more emergently.
- The possibility of aortoenteric fistula should always be considered in patients who have had previous aortic graft surgery and who present with gastrointestinal bleeding because aortoenteric fistula is life-threatening, with a mortality rate of 50% even with surgical intervention. When there is a high degree of suspicion for an aortoenteric fistula, CT with intravenous contrast should be performed before endoscopy or other types of gastrointestinal evaluation.
- patients with no NSAID or H pylori infection and still has idiopathic peptic ulcer disease should continue on qd PPI indefinitely because of high risk for recurring
Endoscopy
- High risk lesions for recurrent bleeding:
- actively bleeding ulcer
- ulcer with nonbleeding visible vessels
- ulcers with clot
- IV PPI for 72 hours to reduce risk for rebleed and remain in hospital
- discharge on BID PO PPI for 2 weeks
- low risk rebleed:
- clean based ulcers
- ulcers with pigmented spots
- mallory weiss tears
- can feed in 24 hours, start qd PPI PO, discharge home
others

reglan: move clots out of the way