ulcerative colitis flare
- related: GI
- tags: #GI
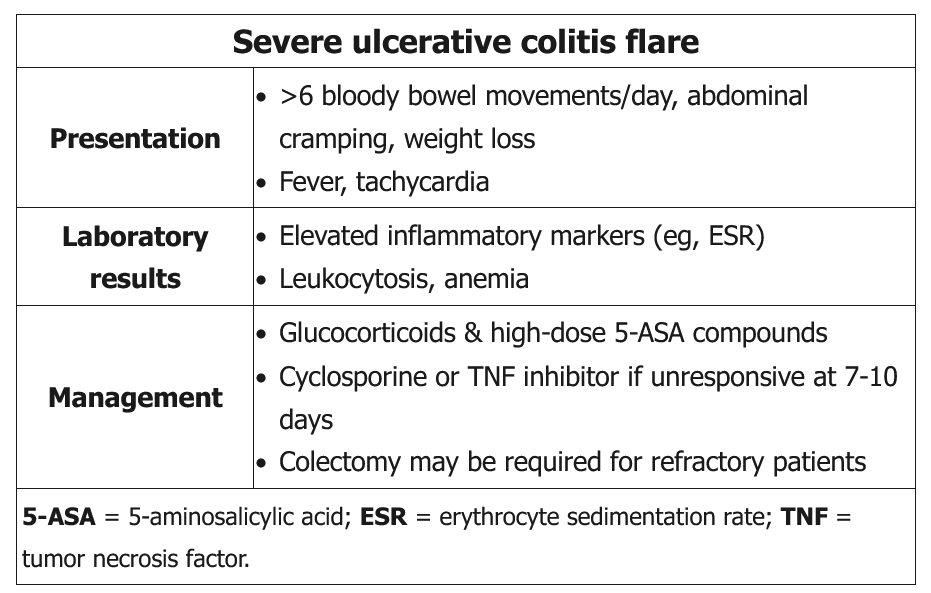
This patient has an acute severe ulcerative colitis (UC) flare, characterized by >6 bloody bowel movements per day, severe abdominal cramps, weight loss, tachycardia, fever, anemia, and elevated inflammatory markers (eg, erythrocyte sedimentation rate). The initial evaluation should include stool studies to rule out infectious colitis (culture, ova, and parasite; Clostridium difficile toxin), flexible sigmoidoscopy to evaluate the extent of disease, and examination for signs of toxic megacolon or colonic perforation.
Management of a severe UC flare includes systemic glucocorticoids and high-dose 5-aminosalicylic acid (5-ASA) compounds. Treatment should not be withheld while awaiting the results of stool studies due to the risk of developing toxic megacolon. Empiric antibiotics (ciprofloxacin/metronidazole) are recommended in severe UC flares only if the patient has signs of severe systemic toxicity (high fevers, marked leukocytosis with left shift and bandemia), evidence of toxic megacolon, or peritonitis (Choice D).
Patients are assessed for response to treatment after 3-5 days. Those with a complete response can transition to oral corticosteroids, but those who fail to respond after 7-10 days of therapy are considered steroid refractory and require either cyclosporine or a tumor necrosis factor inhibitor (eg, infliximab) (Choice A). Those who remain refractory usually require colectomy.
Colonoscopy is avoided during a severe ulcerative colitis flare due to the increased risk of toxic megacolon.
Abdominal CT scan is useful for evaluation of toxic megacolon or perforation, but is not indicated in this patient as physical examination and x-rays are unremarkable. In addition, CT scans should be limited in UC patients due to the cumulative lifetime radiation dose from frequent scans.