triglyceride induced pancreatitis
- related: GI
- tags: #GI
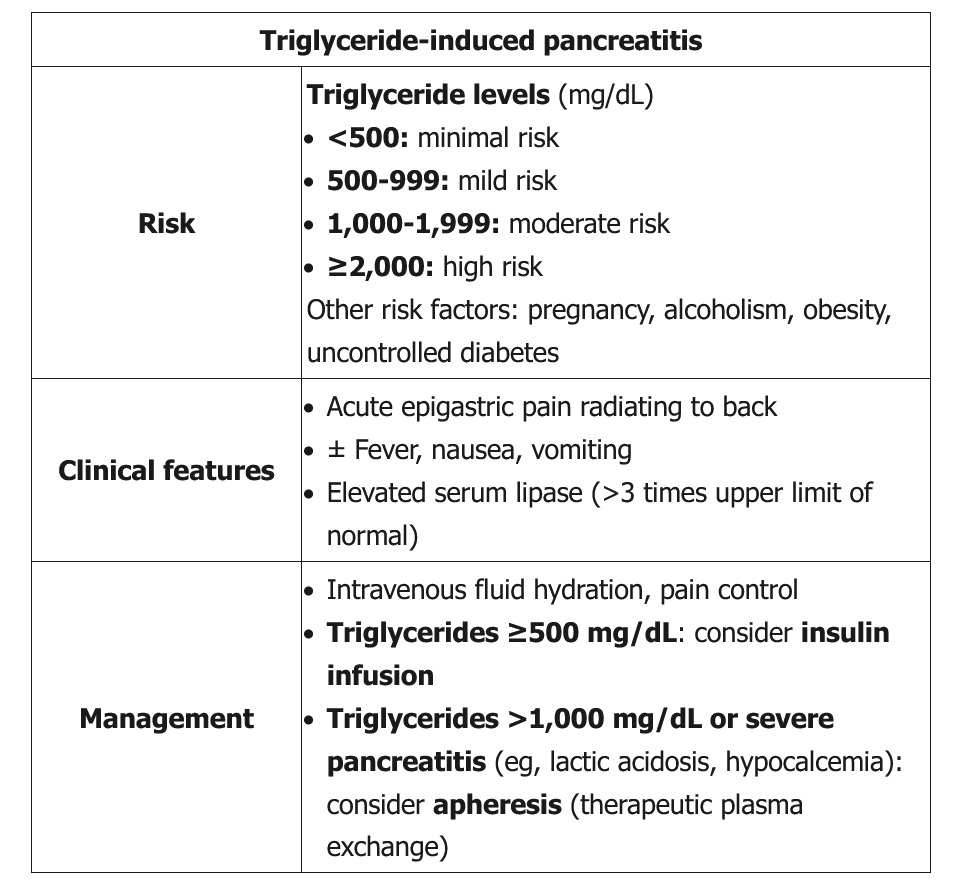
This patient has acute pancreatitis, likely due to hypertriglyceridemia. Pancreatitis can occur in primary (inherited) or acquired hypertriglyceridemia, and the risk increases with pregnancy, alcohol intake, obesity, and uncontrolled diabetes. The risk also increases across all levels of hypertriglyceridemia, but most cases occur in patients with visibly lipemic serum and triglyceride levels >1,000 mg/dL.
Initial management is similar to that for pancreatitis from other causes and includes supportive care (eg, intravenous hydration, pain control). In addition, moderate to severe hypertriglyceridemia-induced pancreatitis (eg, triglycerides >1,000 mg/dL, lipase ≥>3 times the upper limit of normal, evidence of organ dysfunction) requires rapid lowering of serum triglyceride levels:
- If triglyceride levels are >1,000 mg/dL or pancreatitis is severe (eg, lactic acidosis, acute kidney injury, hypocalcemia), as in this patient, **therapeutic plasma exchange (apheresis)__ should be considered to quickly lower triglyceride levels.
- If triglyceride levels are ≥500 mg/dL, an insulin infusion (with intravenous glucose to prevent hypoglycemia when glucose falls below 200 mg/dL) can correct triglyceride levels within 3-4 days by enhancing lipoprotein lipase activity.
Insulin infusion can also be used if plasma exchange is unavailable or not tolerated.
Ultrafiltration and hemodialysis do not remove larger molecules and lipoproteins and therefore are not useful in this patient.
Mild triglyceride-induced pancreatitis (ie, triglycerides <1,000 mg/dL, lipase ≤3 times the upper limit of normal, normal calcium level, no evidence of end-organ damage) can sometimes be managed conservatively, and triglyceride levels fall gradually while the patient is fasting. However, this patient has clinical features (eg, hypocalcemia, acute kidney injury) that warrant more aggressive management.
Once the patient's condition has been stabilized, long-term management should include dietary fat restriction and triglyceride-lowering medication (eg, gemfibrozil). However, these medications would not lower lipids rapidly enough to avoid further pancreatic injury.