transverse mylelitis
- related: Neurology, cauda equina syndrome
- tags: #neurology
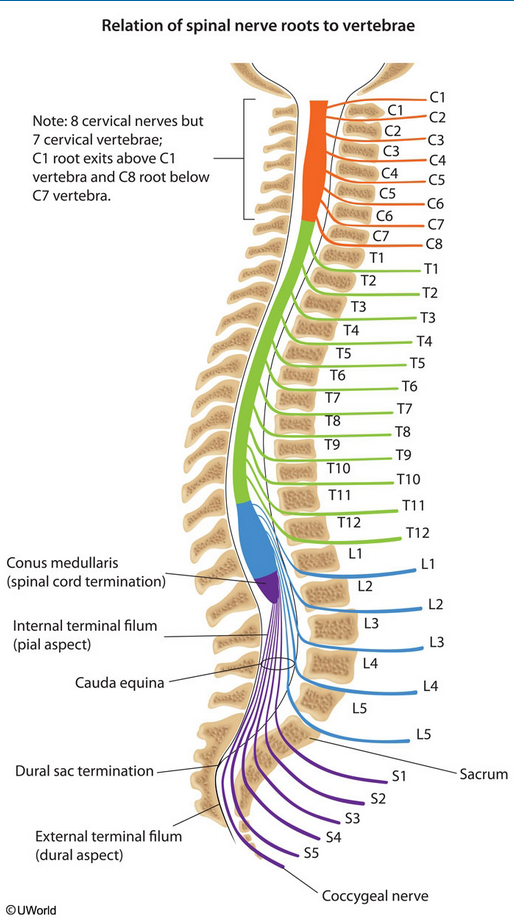
Transverse myelitis is an inflammation of the spinal cord. The term myelitis refers to inflammation of the spinal cord; transverse refers to the pattern of changes in sensation—there is often a band-like sensation across the trunk of the body, with sensory changes below.
Causes of transverse myelitis include infections, immune system disorders, and other disorders that may damage or destroy myelin, the fatty white insulating substance that covers nerve cell fibers. Symptoms include pain, sensory problems, weakness in the legs and possibly the arms, and bladder and bowel problems. The symptoms may develop suddenly (over a period of hours) or over days or weeks.
Patients present initially with spinal shock - lower-extremity weakness, flaccidity, areflexia, and absent Babinski sign. There will be a sensory level to all primary sensory modalities. Bowel and bladder dysfunction are present. Some patients also complain of a "band-like" squeezing pain. After 1 week, patients usually develop spasticity, hyperreflexia, Babinski sign, and clonus.
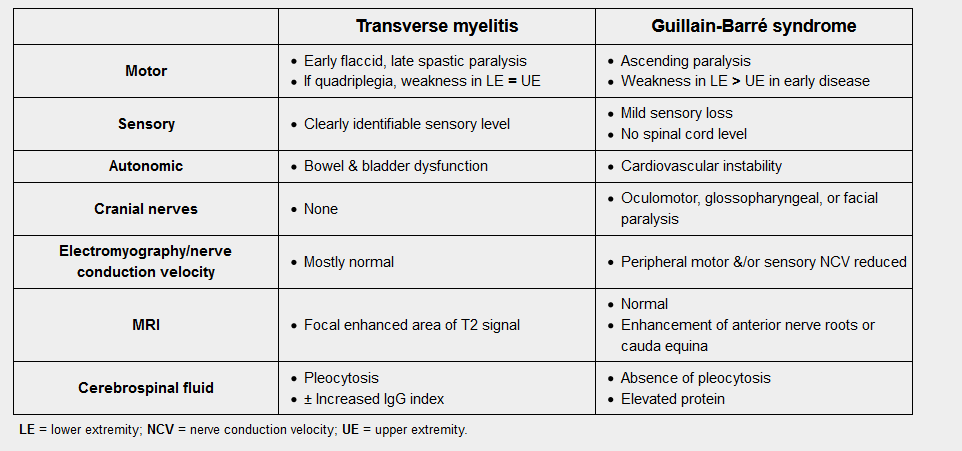
This patient has a rapidly developing myelopathy as evidenced by flaccid paralysis and paresthesias, along with a clearly demarcated sensory level at the umbilicus. Flaccid paralysis and hyporeflexia with a history of upper respiratory infection (URI) may also suggest Guillain-Barré syndrome (GBS). However, a sensory level and bowel/bladder dysfunction after a URI make transverse myelitis (TM) more likely. Patients with GBS will not have bowel/bladder symptoms or a sensory loss below a spinal cord segment. Flaccid paralysis and hyporeflexia are common in early stages of myelopathy (spinal shock).
MRI with contrast is necessary to diagnose the cause of acute myelopathy. In the absence of overt trauma or history of malignancy, compressive lesions such as tumor, herniated intervertebral disk, and epidural abscess are less likely but must still be ruled out. In addition, MRI will show enhancement of the affected spinal cord regions with gadolinium in TM. Three to five days of high-dose corticosteroids should be given once TM is diagnosed. Empiric steroids may be given if there is high suspicion of compressive myelopathy in the setting of malignancy. Recovery usually occurs within 3 months, with up to 40% of patients experiencing some residual disability.
A 26-year-old Caucasian male presents to the emergency department with a three day history of dull back pain, progressive difficulty in walking, and urinary retention. He had a mild upper respiratory infection one week ago, but he is otherwise healthy. He is not taking any medications and denies drug abuse. His temperature is 36.7 C (98 F), blood pressure is 120/76 mmHg, pulse is 80/min, and respirations are 16/min. Neurologic examination reveals a decreased muscle strength (2/5) bilaterally in the lower extremities, hyporeactive knee and ankle reflexes, and decreased pain sensation up to the umbilical level. Which of the following is the most likely diagnosis of this patient?