tia triansient ischemic attack
TIA is characterized by a temporary focal neurologic deficit with an absence of infarction on neurologic imaging. Similar to those of acute ischemic stroke, symptoms of TIA include hemiparesis, mono-ocular or visual field loss, dysarthria, aphasia, and sensory loss. The presence of paresthesia, isolated dizziness or vertigo, or memory loss is more consistent with migraine or seizure. Patients with TIA are at high risk of stroke within the first 48 hours after symptom onset and should be evaluated promptly.
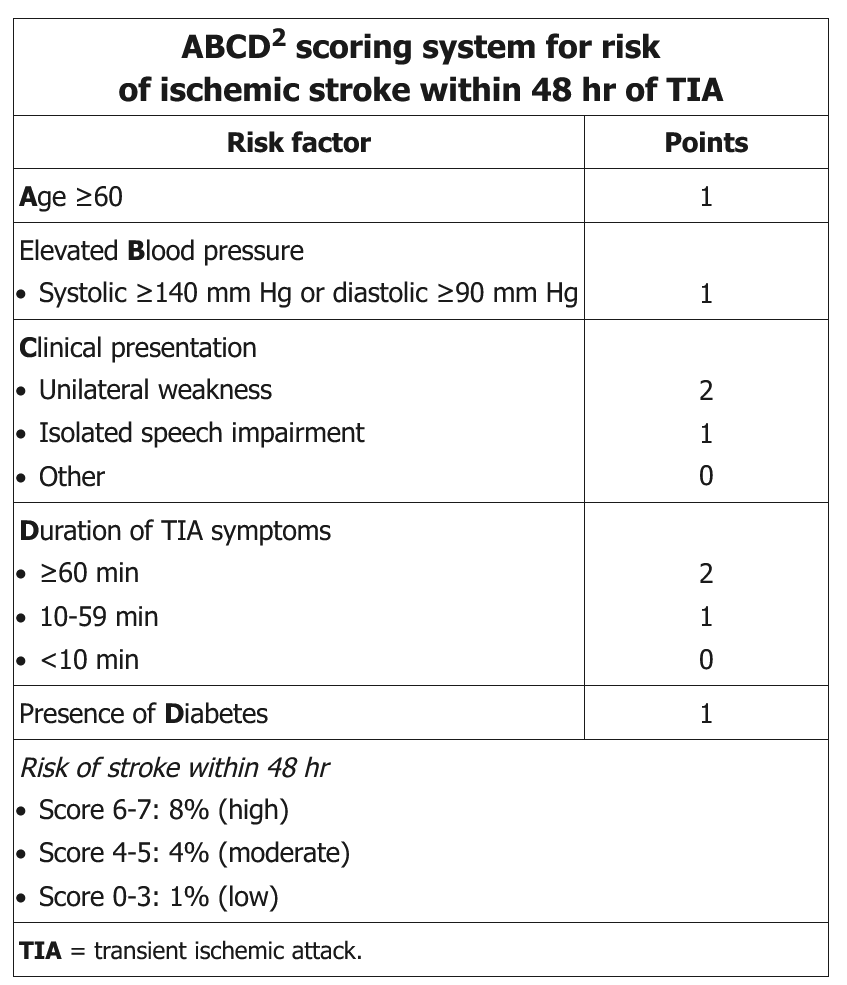
Several post-TIA stroke prediction scoring systems have been developed, with the most widely used being the ABCD2 score, which is based on Age, Blood pressure, Clinical presentation, Duration of symptoms, and the presence of Diabetes mellitus (Table 24). TIA scoring systems, however, do not identify with sufficient sensitivity the highest-risk patients for whom treatment can ameliorate the risk of stroke.
Patients with high-grade extracranial internal carotid artery (ICA) stenosis who have a TIA in a downstream neurologic territory have the greatest short-term risk of stroke. This risk is highest within 2 weeks of TIA for those with greater than 70% stenosis, although 50% to 70% stenosis also carries significant associated risk. In the long term, the risk of stroke is high among patients with atrial fibrillation or other cardioembolic sources requiring anticoagulation.
Management
The National Stroke Association recommends hospitalization for all patients with a first TIA within the last 24-48 hours and the following conditions:
- Duration of symptoms > 1 hour
- Symptomatic internal carotid artery stenosis > 50%
- Multiple recurrent TIAs
- Atrial fibrillation or other known cardiac source of embolus
- Hypercoagulable state
- High risk of stroke after TIA as determined by the ABCD2 score
Preventive therapy (eg, aspirin, statin) is recommended for patients such as this with recent (< 2 weeks) TIA.
Expedited vascular imaging of the ICA and cardiac evaluation for atrial fibrillation are required for all patients with TIA. The initial test of choice for evaluating ICA stenosis is duplex ultrasonography because of its wide availability, low cost, and low risk; if high-grade ICA stenosis is detected and the patient is a candidate for surgery or stenting, confirmatory testing with CTA or MRA is required before intervention. Cardiac evaluation should include electrocardiography for atrial fibrillation, which may be followed by longer-term monitoring. Echocardiography is performed if there is a clinical suspicion of a cardioembolic source or structural heart disease.