Testicular cancer
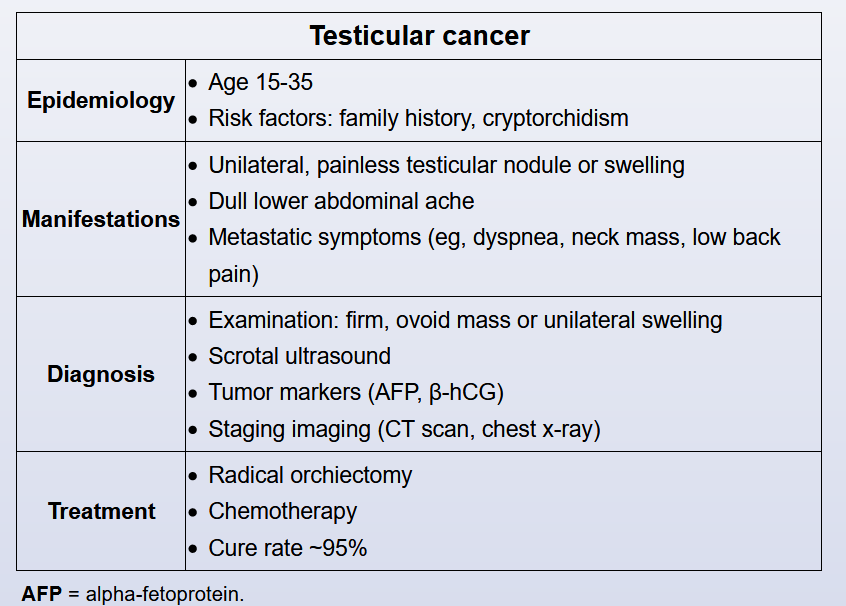
This patient’s presentation is concerning for testicular cancer. The majority (95%) of testicular cancers are germ cell tumors (GCT), which are further divided into seminomas and non-seminomatous tumors. Testicular malignancies classically present as painless scrotal swelling.
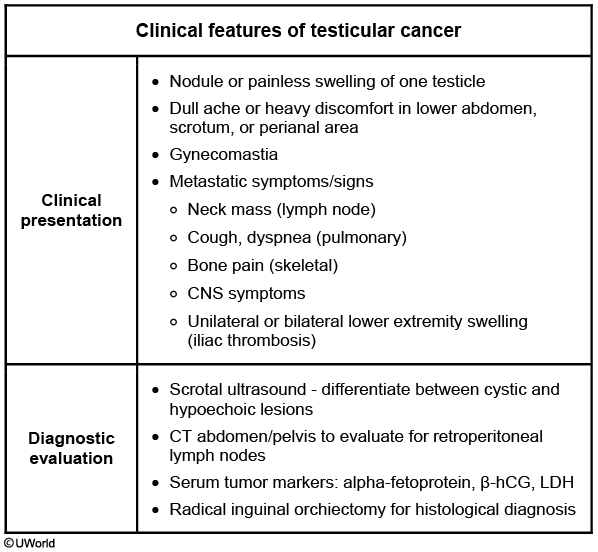
Patients with suspected testicular cancer on physical examination should undergo testicular ultrasound to differentiate cystic from hypoechoic (more likely malignant) lesions. In addition, ultrasound can also rule out hydrocele or epididymitis. After the ultrasound, a staging work-up should be performed. A CT scan of the abdomen and pelvis is required in all patients since testicular cancer initially spreads to the regional retroperitoneal lymph nodes. In addition, a chest x-ray and tumor markers should also be obtained. Non-seminomas typically have elevated AFP and/or β-hCG. Pure seminomas may have elevated β-hCG, but AFP is usually not elevated. Thus, these tumor markers either alone or in combination are insufficient to establish a diagnosis of testicular cancer.
Definitive diagnosis and histology is confirmed by inguinal orchiectomy. Biopsy procedures (e.g., fine needle aspiration, incisional biopsy) are contraindicated due to the risk of local seeding and poorer outcomes (Choices A and B). Histologic distinction is important, since the treatment differs for seminomas (usually chemotherapy and/or radiation therapy) and non-seminomas (usually chemotherapy).
This patient has a firm, uniformly enlarged testicle that does not transilluminate, raising concern for testicular cancer.
Testicular cancer is the most common solid tumor in men age 15-35. Risk is greatest in those with cryptorchidism, but individuals with HIV are at slightly elevated risk. Most patients have painless, unilateral testicular enlargement. Examination usually reveals a firm, hard testicle, with or without nodules, that does not transilluminate.
The initial test of choice for evaluating a testicular mass is bilateral scrotal ultrasound. If ultrasound reveals a solid lesion, further work-up with serum tumor markers (eg, alpha-fetoprotein, β-hCG) and screening CT scans is typically required. Most patients then undergo radical inguinal orchiectomy to establish a tissue diagnosis. Radical orchiectomy plus chemotherapy is usually curative; 5-year survival rates are approximately 95%.