Syphillis
- related: ID
- tags: #id
Congenital
Treponema pallidum crosses the placenta; a syphilis infection during pregnancy can result in vertical transmission, leading to adverse fetal outcomes including fetal growth restriction, intrauterine fetal demise, and congenital syphilis (eg, hepatomegaly, jaundice, rash, skeletal abnormalities).
Diagnosis
The diagnosis of primary syphilis can be made on the basis of dark-field examination of material from a suspect lesion. Serologic test results may be negative in early primary infection.
Diagnosis of secondary and tertiary syphilis relies on serologic testing. Many laboratories use the “reverse” serologic testing strategy, starting with an automated enzyme immunoassay followed by a nonspecific test (rapid plasma reagin or Venereal Disease Research Lab test). Patients with a positive enzyme immunoassay result but negative rapid plasma reagin or Venereal Disease Research Lab test result should have a second specific treponemal antibody test to confirm the result. Those with a confirmed positive result and no history of syphilis treatment should be offered treatment for syphilis of unknown duration.
This woman's serologic results are consistent with successfully treated syphilis, and no additional testing or treatment is indicated. Many laboratories use a “reverse” screening strategy, whereby a treponemal test, such as an enzyme immunoassay (EIA), is performed first and, if positive, is followed by a nontreponemal test (rapid plasma regain RPR or Venereal Disease Research Laboratory VDRL test). If the EIA is positive and the RPR or VDRL is negative, the positive result should be confirmed by a second treponemal test (such as the fluorescent treponemal antibody test performed in this patient). A positive EIA (confirmed by a second test) with a negative RPR is the expected serologic result in a patient who has been treated for syphilis. The treponemal test (EIA) remains positive indefinitely, but the nontreponemal test (RPR or VDRL) should remain negative.
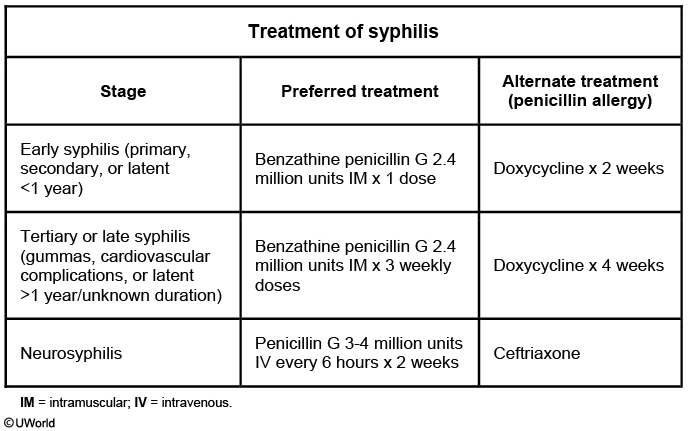
If the nontreponemal test became positive again, it would indicate a new infection, and treatment, based on disease stage, would be indicated. If this patient had reported no history of treatment for syphilis, she should be treated for syphilis of unknown duration, which consists of 3 weekly doses of intramuscular benzathine penicillin. Single-dose benzathine penicillin is indicated for the treatment of primary, secondary, and early latent syphilis.
Because the positive EIA result was already confirmed by a second treponemal test, the fluorescent treponemal antibody, additional testing with another treponemal test, such as the Treponema pallidum particle agglutination assay, is not necessary.
Empiric Treatment
The Centers for Disease Control and Prevention (CDC) guidelines recommend that a patient exposed within 90 days prior to the diagnosis of primary, secondary, or early latent syphilis in a sex partner should receive presumptive treatment (even if the patient is seronegative for syphilis).
A patient exposed >90 days before diagnosis of primary, secondary, or early latent syphilis in a sex partner can undergo serologic testing and treatment accordingly. Presumptive treatment should be given if serologic results are not immediately available or follow-up is uncertain. Long-term sex partners of patients with latent syphilis should also be evaluated with serologic testing and treated appropriately. Although CDC guidelines recommend that nontreponemal tests (eg, rapid plasma reagin) be performed first and that treponemal tests (eg, Treponema pallidum enzyme immunoassay) be used for confirmation, many laboratories have switched the order due to cost-related reasons.
Treatment
This patient's elevated rapid plasma reagin (RPR) titer with positive confirmatory testing by Treponema pallidum enzyme immunoassay indicates syphilis. Because she has no manifestations of primary (eg, chancre) or secondary (eg, rash or aseptic meningitis) syphilis, the patient is classified as having latent syphilis.
Latent syphilis is divided as follows:
- Early latent syphilis is diagnosed when the patient has had syphilis <1 year; this includes patients who had sex for the first time within the past year, had primary or secondary syphilis within the past year, had seroconversion within the past year, or had sex with someone who was showing signs of syphilis within the past year. Early latent syphilis is treated with a single dose of benzathine penicillin G 2.4 million units intramuscularly (also used for primary and secondary syphilis) (Choice B). Doxycycline is sometimes used in place of a single dose of benzathine penicillin in those with severe penicillin allergy (Choice D).
- Late latent syphilis is diagnosed when the duration of infection is unknown (as in this case) or the patient had symptoms or seroconversion ≥1 year ago. Late latent syphilis must be treated with benzathine penicillin G 2.4 million units intramuscularly weekly for 3 weeks. This is typically administered in the outpatient setting.
Without treatment, late latent syphilis can progress to symptomatic tertiary syphilis, leading to cardiac and neurologic complications.
Neurosyphillis
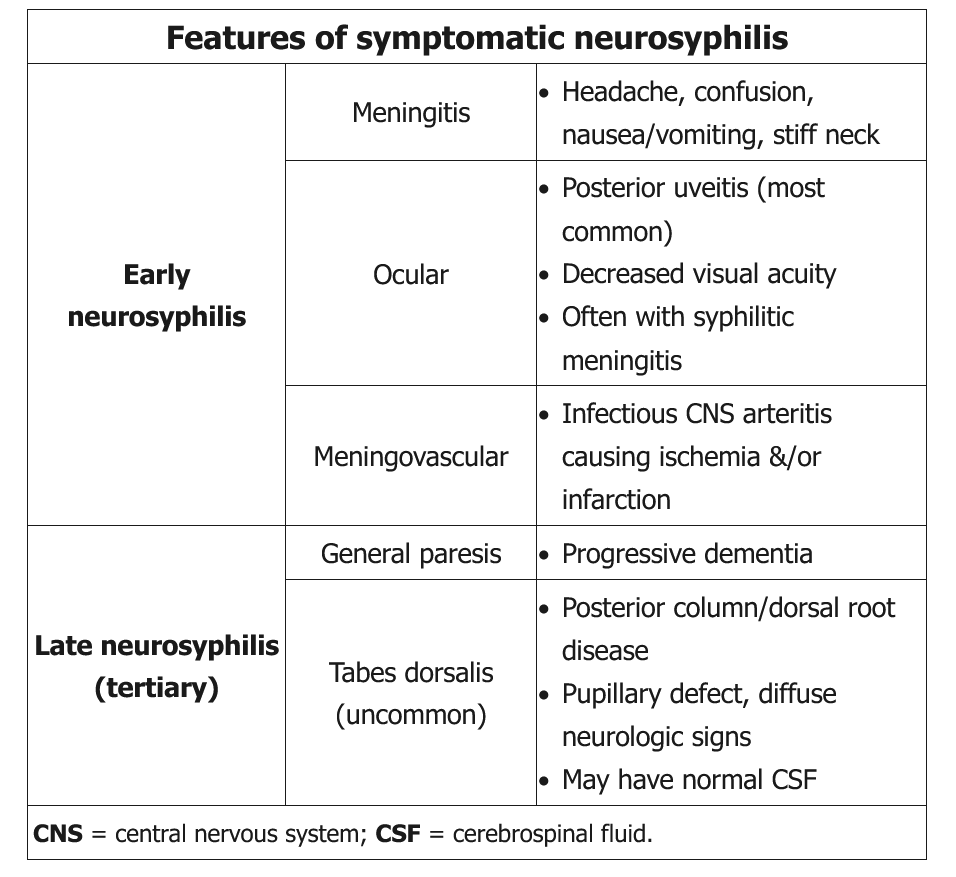
This patient’s presentation is consistent with early neurosyphilis, which can present as various syndromes during any stage of syphilis (summarized in the above table). Neurosyphilis begins with CSF invasion and can cause CSF laboratory abnormalities without clinical symptoms. Patients with neurological symptoms should undergo CSF examination. Cerebrospinal fluid with positive VDRL, lymphocytic pleocytosis, and elevated protein confirms the diagnosis. Since cerebrospinal fluid VDRL may be negative in up to 70% of patients, a positive test is helpful for establishing the diagnosis, but a negative test does not rule out neurosyphilis.
Aqueous intravenous crystalline penicillin G for 10-14 days is the preferred treatment for neurosyphilis. Patients with a possible penicillin allergy should undergo skin testing and desensitization (in consultation with a specialist) if positive. Patients should also undergo serial CSF analysis 3-6 months after treatment and then every 6 months until the CSF shows a normal WBC count and negative VDRL. Patients failing to achieve this after 2 years require retreatment.
Intravenous ceftriaxone is an alternative treatment for neurosyphilis in patients with mild penicillin allergy. Cephalosporins have cross reactivity in penicillin-allergic patients. Thus, administering ceftriaxone is permissible with mild penicillin allergy with careful monitoring; it is not recommended for severe penicillin-allergic patients.
Doxycycline is an alternative therapy for primary or secondary syphilis in patients allergic to penicillin. However, it is not preferred for neurosyphilis unless the patient refuses penicillin desensitization or cannot take ceftriaxone or penicillin.