stable angina
-
related: Cardiology, ACS
-
Definition:
- reproducible angina sx: chest pain/pressure
- at least 2 months
- triggered by stress or exertion
- have not worsened
-
Unstable angina
- new-onset angina or angina at low level exertion
- occur at rest
- accelerating in frequency or severity
-
sx
- classic: tightness, heaviness, gripping chest
- atypical in women/DM: exertional dyspnea
Diagnosis
- step 1: determine pretest likelihood
- baseline ECG to rule out ischemia and guide stress test choice
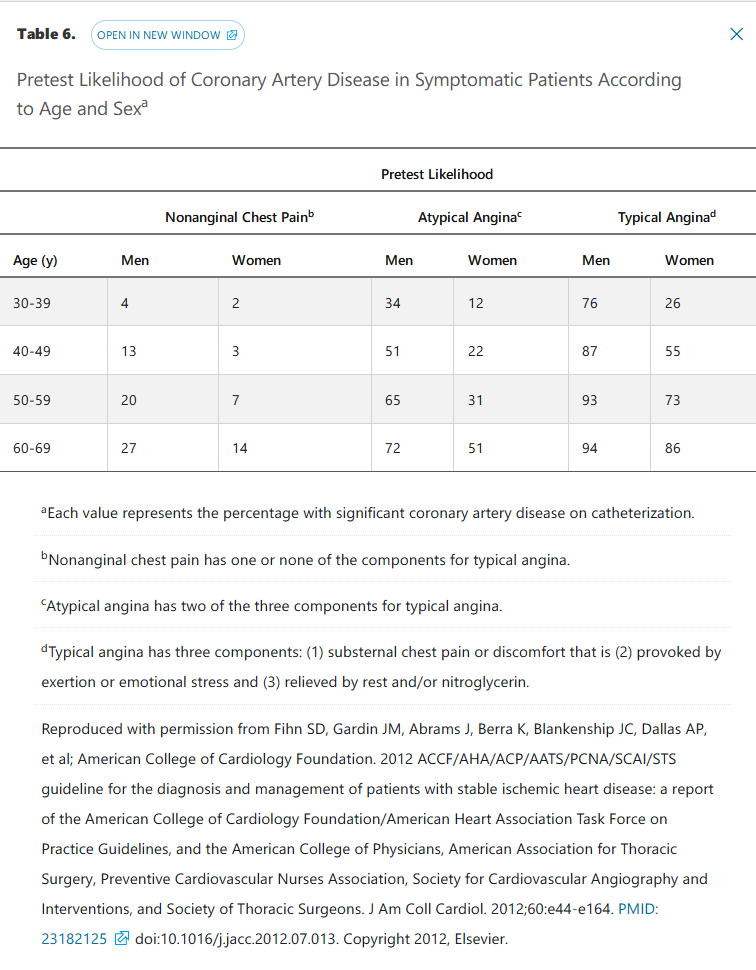
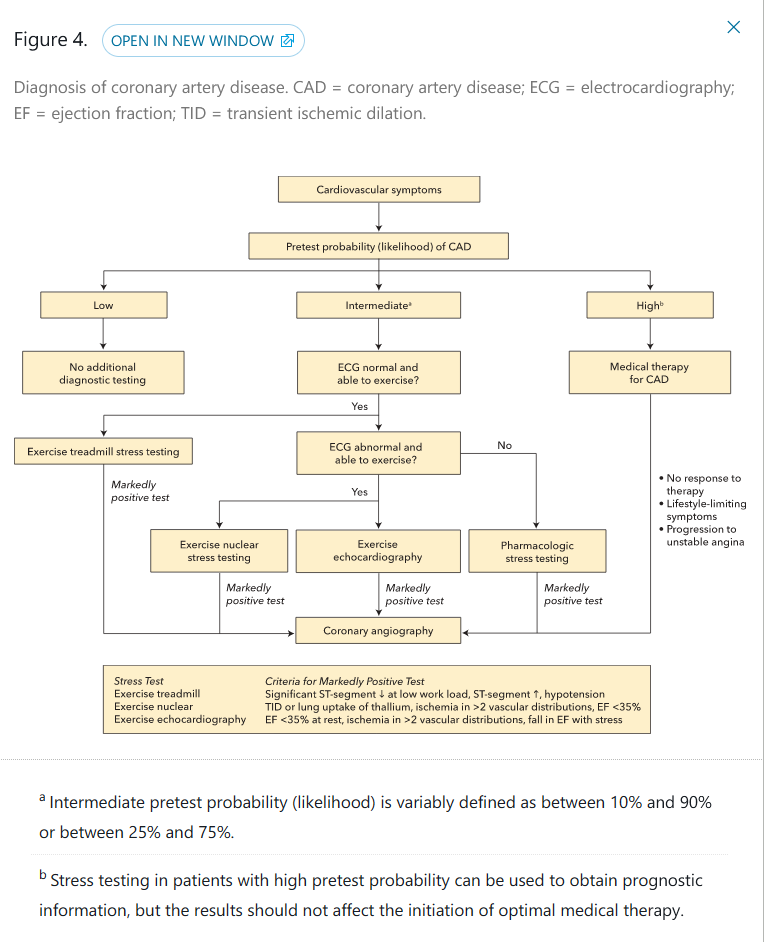
Stress testing is most useful in patients with an intermediate probability of CAD; however, when the pretest probability of CAD is high, testing may provide prognostic information. Other diagnoses should be pursued in patients with normal findings on stress testing. If the stress test yields abnormal results, additional evaluation should be considered.
General Approach to Treatment of Stable Angina Pectoris
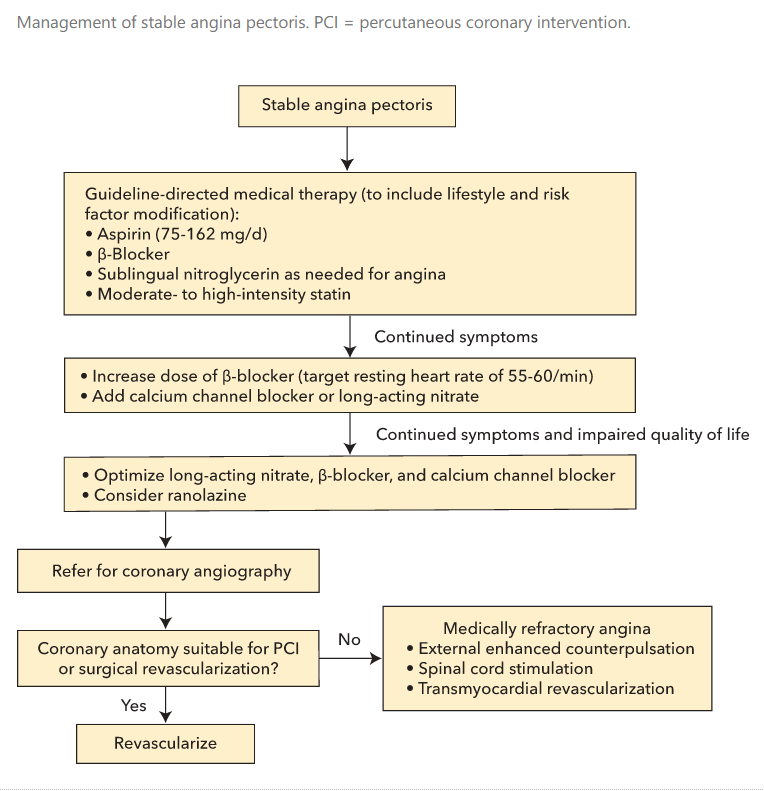
- lifestyle: regular exercise, stop smoking, weight loss, dietary change, blood pressure goal < 130/80, DM control
- cardioprotective meds to halt progression
- antianginal meds reduce cardiac workload, increased myocardial O2 delivery
Cardioprotective Medications
- low dose aspirin
- ASA reduce risk for MI/cardiovascular death in stable angina
- ASA intolerant: use clopidogrel
- prasugrel/ticagrelor has not been studied
- statin
- high intensity lipitor 40-80 or rosuvastatin 20-40
- intolerant: can use statin alternative such as ezetimibe, bile acid sequestrants, fibrates, PCSK 9
- ACE I
- indicated in stable angina if has DM, CKD, HFrEF, hx of MI
Antianginal Medications
- Beta blockers
- first line for stable angina
- lower HR, reduce O2 consumption
- titrate to HR 55-60
- B1 selective such as metoprolol should be used for lung disease pt to avoid worsening respiratory function
- SE: fatigue, lethargy, sleep disturbance, impotence
- CCB
- can be used in addition to BB or intolerant of BB
- vasodilation and reduces vascular resistance, decrease blood pressure, decrease O2 consumption with negative inotrophy
- nondihydropyridine (verapamil, diltiazem): negative chronotropic effect, can worsen heart failure
- short acting dihydropyridine such as nifedipine should be avoided because can worsen acute drop in BP, cause reflex tachyardia and increase demand
- Nitrates
- coronary vasodilation, increase O2 delivery
- decreases preload
- reflex tachycardia
- short acting sublingual should be prescribed as prn
- long acting including isosorbide mono or dinitrate and patch can provide constant vasodilation
- needs to have nitrate-free interval of 12 hours during sleep hours to avoid tolerance
- SE: headache, flushing, hypotension
- do not use with PDE5 inhibitors
- Ranolazine
- decreases angina, increases exercise times
- inhibits Na current, decreases wall tension, O2 consumption, prolongs QT but not proarrhythmic
- typical dose: 1000mg BID, reduce to 500 mg BID in pt receiving CYP meds like verapamil or diltiazem
- avoid in pt with strong CYP drugs: antifungal, HIV meds, clarithromycin
Coronary Revascularization
- consider LHC when sx refractory to medical therapy or abnormal stress test
- angiography with fractional flow reserve test: can provide info on indeterminant lesions. Low flow = significant lesion
- PCI
- no evidence PCI superior to medical therapy in stable CAD
- COURAGE trial and BARI-2D trial: no difference in mortality or MI incidence
- CABG
- for multivessel CAD, also better than PCCI for left main or 3v CAD, also good for pts with DM and left ventricular dysfunction
- STICH trial: survival advantage over PCI in multivessel CAD and LV dysfunction pts
- After revascularization
- needs GDMT
- ASA: indefinite
- BMS: 1 month DAPT
- DES: stable angina, 6 months
- CABG: 12 months