-
Paracentesis
paracentesis
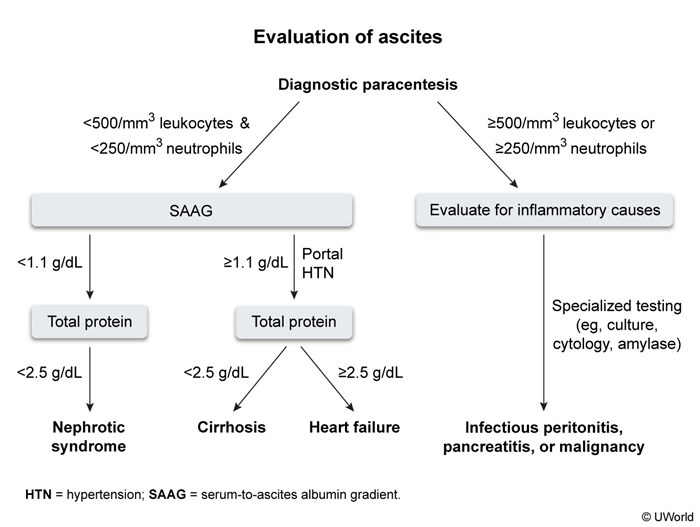
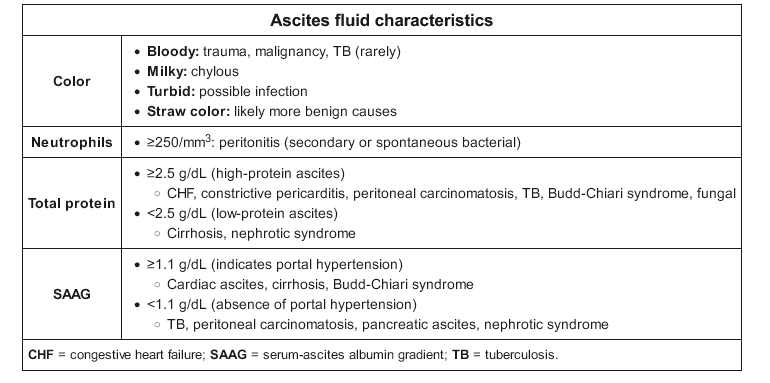
- SAAG > 1.1: portal HTN
- TP > 2.5: cardiac, heart failure, budd chiari
- TP < 2.5: cirrhotic
- if TP < 1.5: less complement, less immunity, assume SBP
- SAAG < 1.1: nephrotic syndrome
- SBP: signs of renal dysfunction, bad systemic function (bili > 3, Child pugh > 9)
- por
- SAAG > 1.1: portal HTN
-
Hepatic Encephalopathy
hepatic encephalopathy
- related: sbp
- tags: #note
- confusion from liver insufficiency or porto-systemic shunting (bypassing liver)
- after tips: 10-50% of overt HE in 1 year
- overt: asterexis and/or disorientation
- ammonia not needed for diagnosis
- no ppx needed in pts who have never had HE
- precipitating factors
-
Peritoneal Dialysis
peritoneal dialysis
- related: Nephrology, sbp
- tags: #nephrology
Peritoneal dialysis utilizes an indwelling catheter to perform exchanges of dialysate with a specified solute concentration and osmolality into the peritoneum, which serves as a semipermeable membrane and allows for diffusion of solutes and osmosis of water. Dialysate needs to be exchanged about three to five times per day to maintain a high concentration gradient and maintain adequate solute