pulmonary hypertension workup
- related: Pulmonology
- tags: #pulmonology
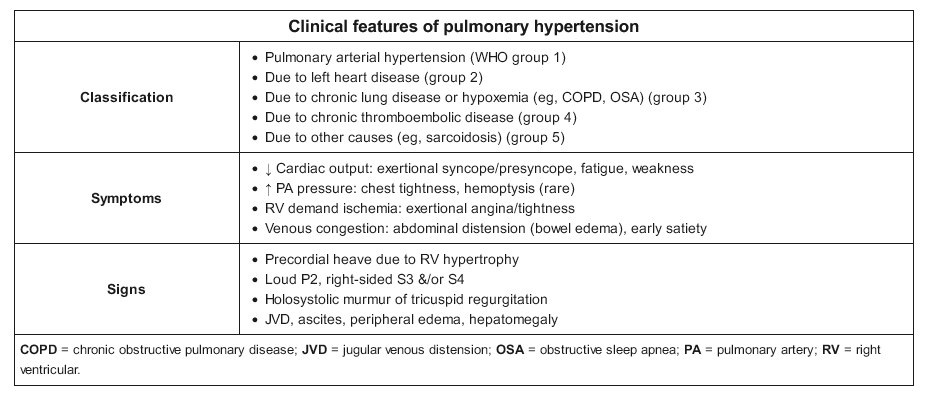
This patient has progressive dyspnea, exercise intolerance, and chronic right ventricular (RV) pressure overload seen on echocardiography (ie, RV hypertrophy, elevated pulmonary artery systolic pressure [PASP]). This presentation is suggestive of pulmonary hypertension (PH).
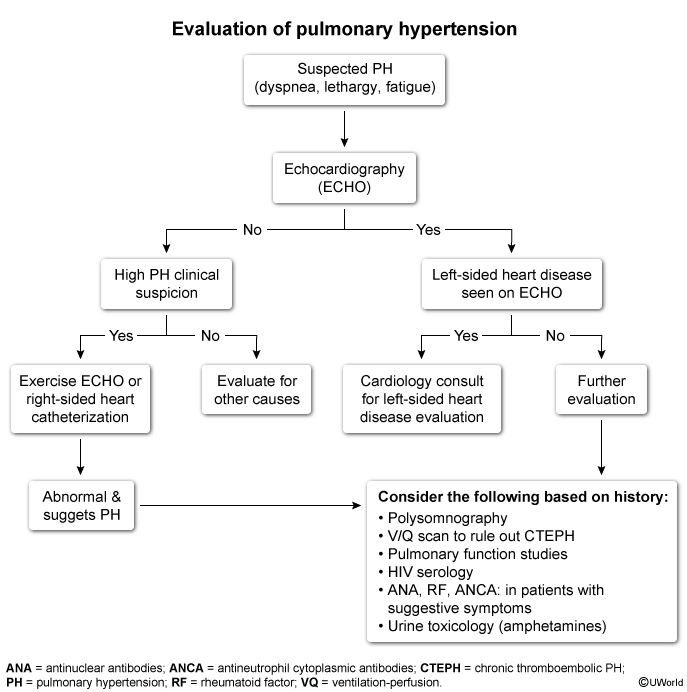
Evaluation of patients with suspected PH begins with resting echocardiography. If PASP is normal but PH remains clinically suspicious, exercise echocardiography can accentuate the hemodynamic changes. If PASP is elevated (eg, ≥50 mm Hg), PH is likely. A thorough history, examination, and select diagnostic tests are performed to ascertain the etiology and classify the PH.
Group 1
Pulmonary arterial hypertension (PAH) (WHO group 1): PAH can be related to certain autoimmune conditions (eg, rheumatoid arthritis, scleroderma). However, isolated pulmonary vascular involvement is exceedingly rare; patients usually have evidence of rheumatism or connective tissue disease (eg, sclerodactyly, Raynaud disease).
Group 2
Left heart disease (group 2): The most common cause of PH in the United States is left-sided heart disease (eg, mitral stenosis, diastolic dysfunction). Significant left-sided heart dysfunction is usually evident on echocardiography.
Right-sided heart catherization, sometimes performed during evaluation of pulmonary hypertension (PH), reveals an abnormally elevated mean pulmonary arterial pressure compatible with PH (39 mm Hg; normal: ≤20). Pulmonary capillary wedge pressure (surrogate for left atrial pressure) is congruently elevated (33 mm Hg; normal: ≤15). Therefore, the patient's PH is proportional to HFpEF, and he likely has postcapillary PH-HFpEF (WHO group 2) from impaired diastolic filling, leading to back pressure on the pulmonary veins. Right atrial pressure and cardiac output are normal, indicating well-compensated right ventricular function, explaining the negligible peripheral edema.
Pulmonary vasodilators (eg, tadalafil, bosentan) are indicated for pulmonary arterial hypertension (WHO group 1), which features prominent vasoconstriction. They are avoided in PH-HFpEF due to the risk of precipitating acute pulmonary edema by suddenly increasing pulmonary blood flow into a stiff/unprepared left ventricle.
Group 3
- Lung disease/hypoxemia (group 3): Patients typically have a preexisting history of lung disease (eg, abnormal spirometry, parenchymal abnormalities on imaging) and/or signs of sleep-disordered breathing (eg, daytime sleepiness, snoring, arousals), which can be evaluated by polysomnography (Choice C).
Group 4
Chronic thromboembolic PH (CTEPH) (group 4): In approximately 2% of patients with acute pulmonary embolism (as in this patient with a history of postoperative pulmonary embolism), the clots become scarred into the vessel wall, leading to chronic vascular obstructions. If present, pulmonary bruits are a very specific sign of CTEPH, reflecting turbulent flow through these irregularly narrowed arteries.
Because pulmonary thromboendarterectomy surgery is potentially curative, a correct diagnosis is essential. Ventilation-perfusion scanning is the test of choice for CTEPH because it is the most sensitive method for detecting distal subsegmental perfusion defects. CT pulmonary angiography is more accurate for visualization of fresh segmental pulmonary emboli but is often obtained in patients with confirmed CTEPH to identify those with favorable operative disease (Choice A).