Prostate Cancer
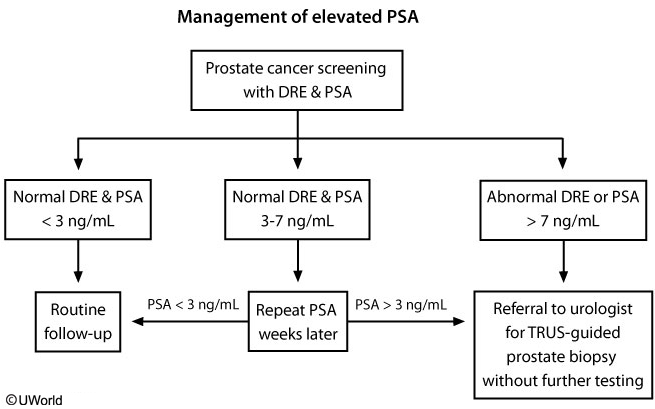
Prostate cancer is widely prevalent in men age >65. Most cases are slow-growing and do not result in death. Risk stratification using digital rectal examination, PSA level, and biopsy with Gleason score can help to determine the optimal treatment approach and prevent unnecessary treatment-related morbidity.
Patients with prostate cancer are generally stratified as very low-risk when the following features are present:
- Gleason score of <6 with <3 cores affected (<50% involvement in each affected core)
- Normal digital rectal examination
- PSA <10 ng/mL
Patients with very low-risk (and many with low-risk) prostate cancer have excellent 10-year survival rates and should be treated with active surveillance rather than definitive therapy. Active surveillance includes monitoring serum PSA levels every 3-6 months, having a digital rectal examination yearly, and having a repeat prostate biopsy at the end of year 1 to ensure that higher-grade disease was not missed on the original biopsy.
Individuals who progress on active surveillance and those with higher initial risk stratifications (moderate, high, very high) are typically treated with radiotherapy or radical prostatectomy. These therapies are associated with high cure rates but often cause significant morbidity. Radiotherapy (eg, brachytherapy, external beam) commonly results in urinary and gastrointestinal irritation as well as erectile dysfunction (Choice C). Radical prostatectomy is associated with high rates of sexual dysfunction and moderate rates of urinary incontinence (Choices A and D).
(Choice B) Androgen deprivation therapy is not generally recommended for localized prostate cancer but is widely used for metastatic prostate cancer. Patients with very low-risk or low-risk prostate cancer are considered to have localized disease and do not require androgen deprivation therapy or evaluation (eg, CT scan, bone scan) for metastatic disease.