plasmodium
- related: ID
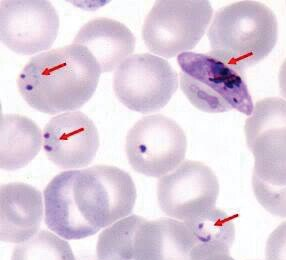
This pregnant woman has contracted Plasmodium falciparum malaria after visiting a part of the world where malaria is endemic. Her clinical presentation and peripheral blood smear showing many parasitized erythrocytes demonstrating signet ring forms, together with the absence of trophozoites and schizonts, are typical for infection with P. falciparum. Of returning travelers with acute and potentially life-threatening febrile diseases, P. falciparum malaria accounts for most infections. Furthermore, pregnant women are at increased risk of severe disease and a heightened mortality rate, which is likely related to a reduced immune response. Additionally, effects on the microvasculature and sequestering of organisms in the placenta during pregnancy are known to significantly increase the risk of miscarriage, premature delivery, low-birth-weight neonates, congenital infection, and fetal demise.
Accurate identification of P. falciparum and Plasmodium knowlesi is critical because of the risk for severe and potentially lethal infection. P. falciparum should be suspected if the patient traveled to Africa, symptoms begin soon after return from an endemic area, and the peripheral blood smear shows a high level of parasitemia. P. knowlesi is a more recently recognized human pathogen; infection may be severe because of high levels of parasitemia. Examination of the peripheral blood smear reveals all stages of the parasite. The epidemiologic history is helpful because P. knowlesi is not encountered in Africa but rather South and Southeast Asia.
Plasmodium malariae, Plasmodium ovale, and Plasmodium vivax are all associated with a low or very low degree of parasitemia, typically less than 2%, and although the risk of recurrence is high, with the exception of P. vivax, the risk for severe disease is low.
A 27-year-old woman is hospitalized with a 5-day history of intermittent fever, headache, muscle pains, and abdominal cramps. She returned 8 days ago from a 1-week trip to Kenya and Tanzania. She spent time outdoors in the evening and went hiking in a wooded park. She is pregnant at 20 weeks' gestation. She declined pretravel immunizations as well as antimalarial chemoprophylaxis. Her only medication is a prenatal vitamin.
On physical examination, temperature is 39.1 °C (102.3 °F), blood pressure is 98/64 mm Hg, pulse rate is 112/min, and respiration rate is 16/min. Her conjunctivae are icteric. Cardiopulmonary examination reveals regular tachycardia. The remainder of the examination is unremarkable.
A peripheral blood smear is shown.
Malaria is transmitted to humans by the female Anopheles mosquito. It is the most common cause of febrile illness in returning travelers, particularly from sub-Saharan Africa and large parts of Asia. Preventive measures include limiting outdoor exposure between dusk and dawn, using insecticide-impregnated bed nets and insect repellents containing 20% N-diethyl-3-methylbensamide (DEET), and using antimalarial chemoprophylaxis.
Incubation periods vary by species and range from 1 week to 3 months in semi-immune persons or those taking inadequate prophylaxis. Symptoms include fever (characteristically paroxysms in 48- or 72-hour cycles), headache, myalgia, and gastrointestinal symptoms. More severe disease occurs with hyperparasitemia (5%-10% parasitized erythrocytes) leading to adherence in small blood vessels causing infarcts, capillary leakage, and multiorgan system dysfunction. Serious disease primarily occurs with Plasmodium falciparum; manifestations include mental status alterations, seizures, hepatic failure, disseminated intravascular coagulation, brisk intravascular hemolysis, metabolic acidosis, kidney disease, hemoglobinuria, and hypoglycemia. Subsequently, patients may develop anemia, thrombocytopenia, splenomegaly, and elevated aminotransferase levels. See Table 43 for specific features of the five Plasmodium species.
Diagnosis is made by identification of malarial parasites on the peripheral blood smear. Morphologic features help determine the specific species. Rapid tests that detect malaria antigens are available but may lack sensitivity and specificity. Polymerase chain reaction (PCR) and serologic assays exist, although each has limitations.
It is critical to identify P. falciparum and P. knowlesi because of their potential for severe infection. The onset of malarial symptoms shortly after returning from travel to endemic zones, such as Africa, and recognition of a high level of parasitemia and distinctive morphologic characteristics (Figure 18) should raise suspicion for P. falciparum infection. P. knowlesi is an emerging human pathogen found in South and Southeast Asia; high levels of parasitemia may occur, and examination of the peripheral blood smear reveals all stages of the parasite.
Malarial chemoprophylaxis and treatment depend on possible drug resistance and individual contraindications to specific medications (Table 44 and Table 45).