perioperative warfarin management
- related: Cardiology, Perioperative
- tags: #cardiology
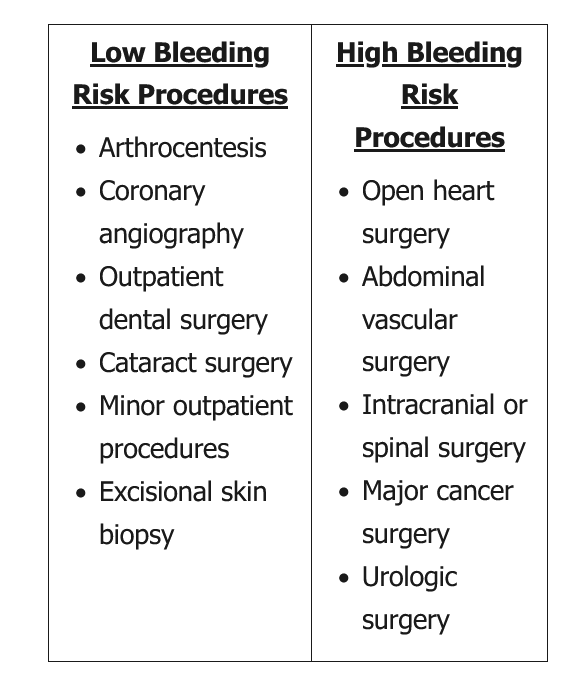
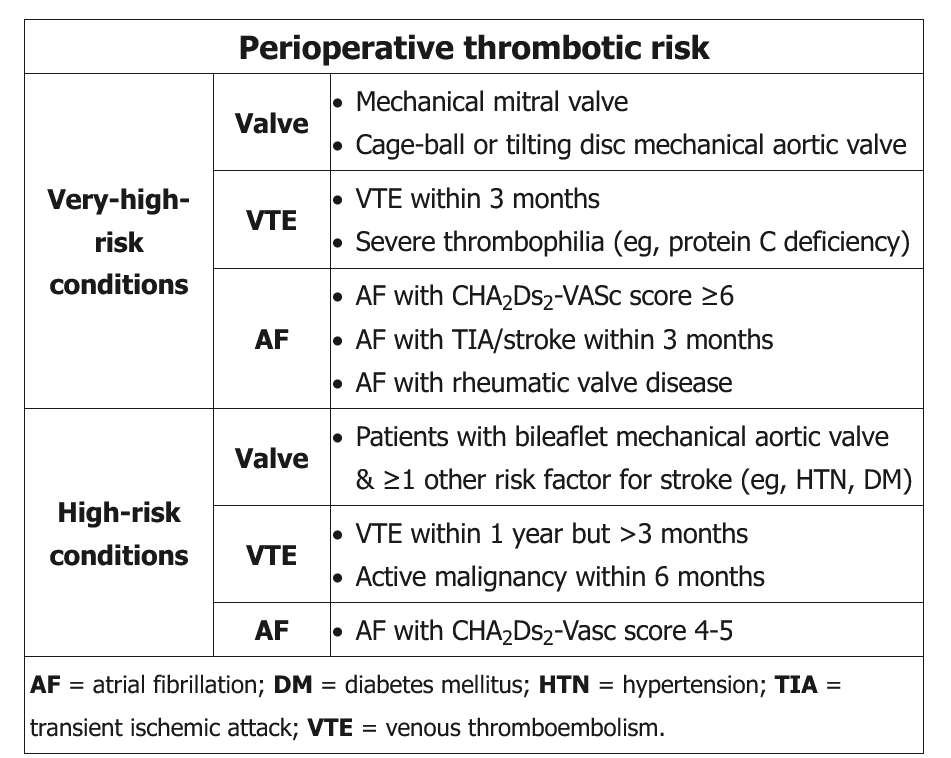
In patients with a mechanical prosthetic valve undergoing elective surgery, the decision to continue or hold warfarin anticoagulation is based on the risk of systemic thromboembolism (risk factors and type/location of prosthetic valve) and the risk of post-procedure bleeding (type of surgery). The presence of a mechanical prosthetic mitral valve puts the patient at a high risk for systemic thromboembolism. In patients undergoing low risk surgical procedures, such as dental extraction, warfarin anticoagulation is associated with a minimal risk of serious bleeding and should be continued through the procedure.
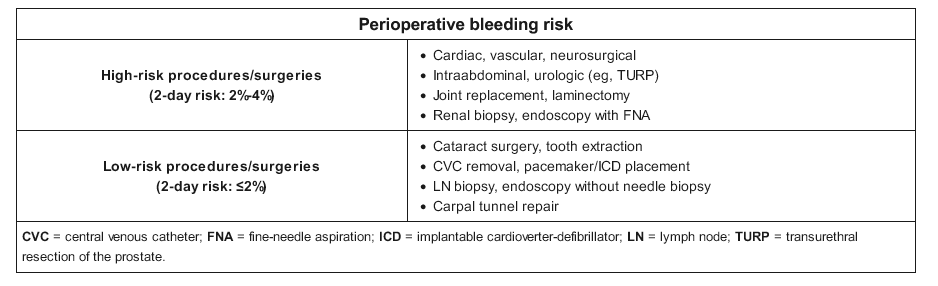
This patient on warfarin due to his mechanical valve is scheduled for a high-bleeding-risk procedure (ie, endoscopic ultrasound with biopsy). A mechanical bileaflet aortic valve is considered either a moderate-thrombotic-risk condition or, when accompanied by ≥1 additional risk factor for stroke (eg, hypertension), a high-thrombotic-risk condition. The generally recommended approach in patients with moderate or high thrombotic risk is to hold warfarin for 5 days until the INR falls <1.5 and then perform the procedure. Warfarin can usually be resumed the evening following the procedure with no need for bridging.
In contrast to the high rate of blood flow through the aortic valve, the relatively stagnant blood flow surrounding the mitral valve creates very high thrombotic risk in patients with a mechanical mitral valve. For patients with a very-high-risk thrombotic condition, perioperative bridging with low-molecular-weight or unfractionated heparin is indicated; warfarin is typically held 5 days prior to the procedure, and heparin is started once the INR is <2.0 (rather than <1.5) (Choice D). Heparin should be stopped the day of the procedure and then restarted 24-48 hours afterward, in combination with warfarin, when adequate hemostasis has been achieved.
Patients undergoing low-bleeding-risk procedures (eg, carpal tunnel repair, tooth extraction, endoscopy without biopsy) can often proceed without any change in anticoagulation regimen.
https://pubmed.ncbi.nlm.nih.gov/18574269/ https://pubmed.ncbi.nlm.nih.gov/12719198/