perforated peptic ulcer
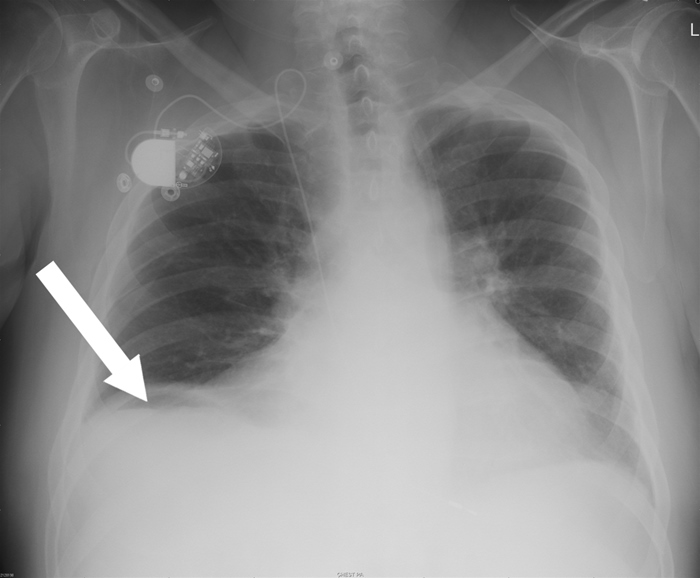
This patient's acute abdominal pain with significant tenderness and guarding is highly suggestive of bowel perforation with peritonitis. A perforated peptic ulcer is the most common etiology, and is especially likely in this patient who has a history of "burning" abdominal sensations. In contrast to patients with renal colic, who tend to writhe in pain, patients with peritonitis tend to lie flat and motionless to limit peritoneum irritation. Rupture of a hollow organ allows air into the abdomen (pneumoperitoneum); this air can often be detected by an upright chest x-ray. It is important to keep the patient in an upright position so that air within the peritoneal cavity can be visualized beneath the diaphragm. Pneumoperitoneum identification in a supine patient can be much more difficult. Given this patient's presentation, the presence of pneumoperitoneum on the chest x-ray would likely be diagnostic. If the findings of the chest x-ray are unclear, an abdominal CT scan may be useful (Choice C).
Peptic ulcer perforation is a potentially fatal complication of peptic ulcer disease. If left untreated, the patient can have a rapid clinical deterioration leading to death within 12-24 hours. However, early diagnosis and treatment generally lead to excellent prognosis and most patients recover fully. Emergency surgery (open or laparoscopic) is indicated in all patients with perforated peptic ulcer.
In preparation for surgery, patients with a perforated viscus should receive fluid resuscitation and broad-spectrum intravenous antibiotics with good coverage for Gram-negative organisms. Intravenous proton-pump inhibitor therapy is also suggested for patients with perforated peptic ulcer.