parkinsons
- related: Geriatrics
- tags: #note
Most medications for Parkinson disease increase dopamine activity, either through direct receptor stimulation (eg, dopamine agonists, carbidopa/levodopa), decreased dopamine breakdown (eg, monoamine oxidase [MAO-B] inhibitors), or increased dopamine release (eg, amantadine). Other medications include anticholinergics (which can decrease acetylcholine effect in relation to dopamine effect) and catechol-O-methyl transferase (COMT) inhibitors, which can prolong levodopa's effect. Any medication that increases dopamine activity can cause psychotic symptoms. This patient has developed paranoid delusions and visual hallucinations following an increase in levodopa. Although dosage reduction or discontinuation of carbidopa/levodopa is an option (Choice D), this would not be the appropriate first step as this medication has significantly improved the patient's motor symptoms and quality of life. To maintain therapeutic effect, the least potent medications should be reduced or discontinued first, in the following order: anticholinergics, amantadine, MAO-B inhibitors, COMT inhibitors, dopamine agonists, and, finally, carbidopa/levodopa. The first step would be to reduce or taper off amantadine while maintaining the dosage of carbidopa/levodopa.
Addition of low-dosage antipsychotics is indicated for medication-induced psychosis that persists despite adjustments to determine the minimum effective dosage of anti-parkinsonian medication. The low-potency second-generation antipsychotics quetiapine (Choice A) and clozapine have the lowest incidence of drug-induced parkinsonism and may be indicated. In contrast, potent D2 dopamine receptor antagonists such as first-generation antipsychotics and the second-generation antipsychotic risperidone (Choice B) should be avoided due to the risk of motor symptoms. Recently, pimavanserin, a serotonin 5HT-2A receptor inverse agonist, has been approved by the FDA for the treatment of psychotic symptoms in patients with Parkinson disease.
Early Parkinson's
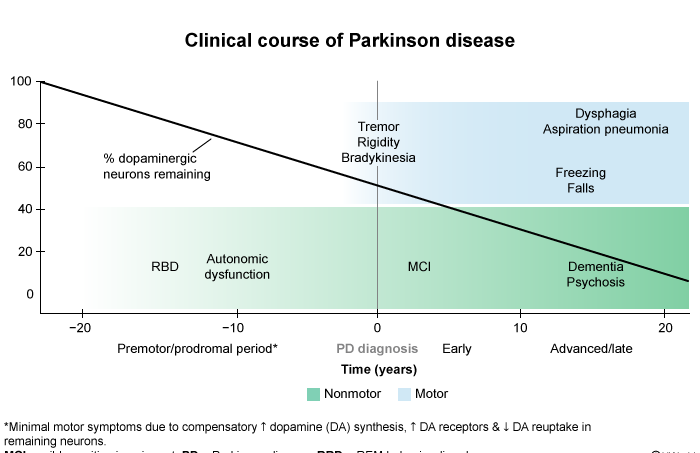 This patient has nonmotor symptoms of early idiopathic Parkinson disease (PD). PD is uncommon in patients age <40. Certain nonmotor symptoms can be seen years before the onset of motor symptoms (ie, bradykinesia, rigidity, tremor) and could suggest early PD. These include issues with sleep, excessive daytime somnolence, mood disturbance, anosmia, and constipation, as seen in this patient. Depression and anxiety can also be seen in up to 50% of patients and are thought to be some of the most troublesome nonmotor symptoms.
This patient has nonmotor symptoms of early idiopathic Parkinson disease (PD). PD is uncommon in patients age <40. Certain nonmotor symptoms can be seen years before the onset of motor symptoms (ie, bradykinesia, rigidity, tremor) and could suggest early PD. These include issues with sleep, excessive daytime somnolence, mood disturbance, anosmia, and constipation, as seen in this patient. Depression and anxiety can also be seen in up to 50% of patients and are thought to be some of the most troublesome nonmotor symptoms.
Rapid eye movement (REM) sleep behavior disorder is seen in approximately 15%-47% of patients with PD and is characterized by dream-enacting behaviors such as talking, yelling, punching, kicking, and jumping from bed. More than 75% of patients with spontaneous REM sleep behavior disorder subsequently develop PD or other alpha-synucleinopathies (eg, dementia with Lewy bodies).