neisseria meningitis
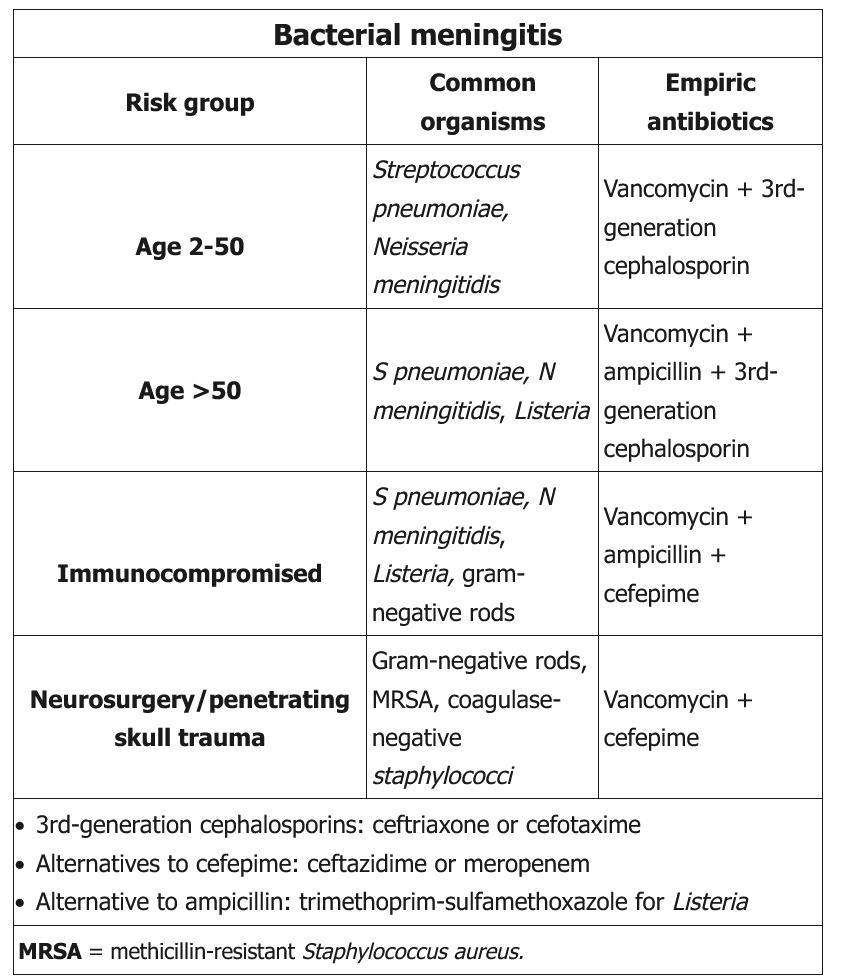
Neisseria meningitidis is the most common cause of acute bacterial meningitis in children and adolescents age 2-18. N meningitidis attaches to the nasopharyngeal epithelium, where it can replicate asymptomatically or cause invasive disease. Mucosal invasion is followed by bacteremia, leading to sepsis, meningitis, or both.
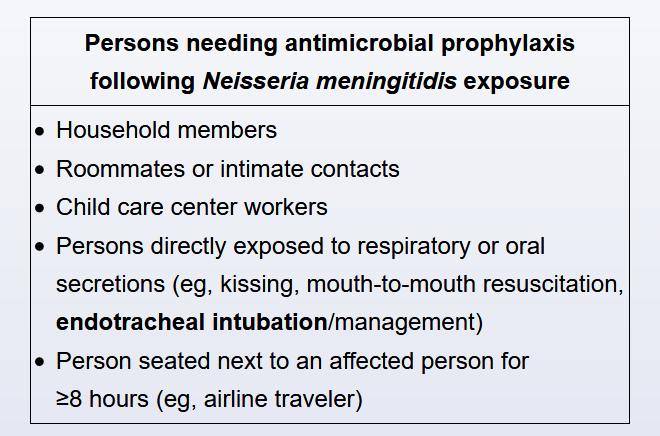
Meningococcal meningitis is a devastating illness associated with significant morbidity and mortality. Antibiotic chemoprophylaxis can prevent its spread and is indicated for high-risk contacts. These include those who live in the same household or who have had prolonged, close contact with a patient and his or her secretions (eg, roommates, significant others). In addition, all health care workers who have had direct exposure to the patient's respiratory secretions (ie, during suctioning or intubation) should receive chemoprophylaxis. Finally, child care workers require prophylaxis due to the increased risk of exposure to the saliva of a pre-school aged child.
Low-risk contacts do not require antibiotic prophylaxis. These include casual contacts (such as co-workers, classmates, or teachers) and health care providers who were briefly exposed to the patient but had no direct contact with secretions (eg, the paramedic who drove the ambulance and the emergency department staff who were not involved in this patient's care). Individuals who have direct contact with a high-risk contact but not the patient are also considered low-risk (eg, the babysitter of a patient's younger sibling).
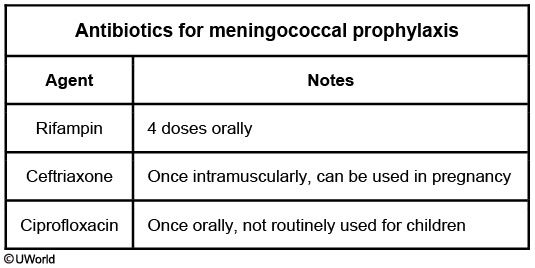
Antibiotic chemoprophylaxis is used to decolonize close contacts of patients with meningococcal meningitis, as they may carry the same invasive strain. To prevent secondary cases, selected agents need to be highly efficacious and easy to adhere to. Oral rifampin (every 12 hours for a total of 4 doses) is the recommended regimen. Ciprofloxacin and intramuscular ceftriaxone can also be used. Other antibiotics are either less effective or more difficult to administer.