myasthenia crisis
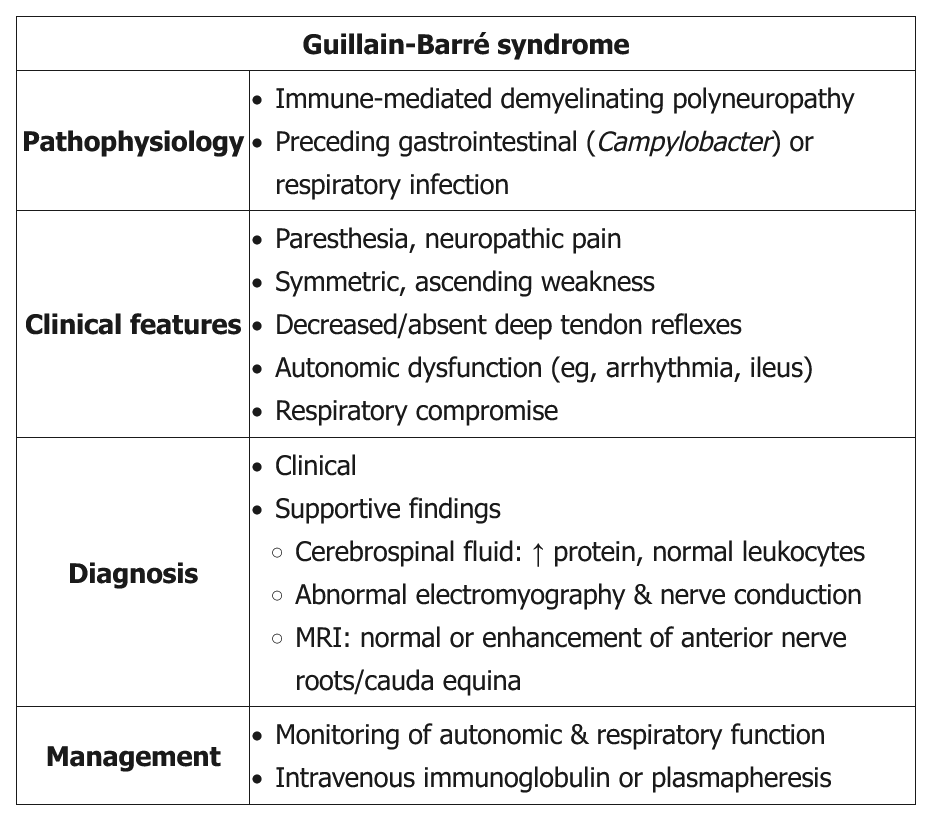
- related: Neurology, gbs guillain barre syndrome
- tags: #neurology
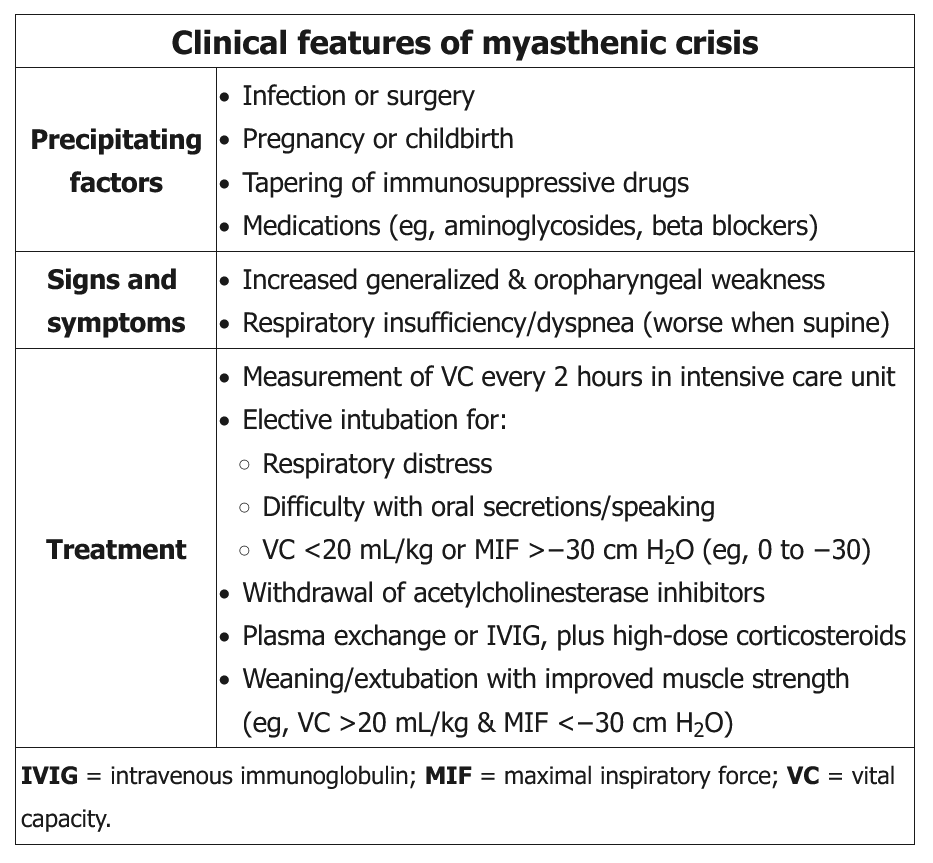
This patient's presentation is consistent with myasthenic crisis, defined as severe weakness from myasthenia gravis requiring intubation. Myasthenic crisis is usually due to weakness of the respiratory muscles but can also present as severe oropharyngeal weakness resulting in dysphagia and aspiration. The common precipitants are infection and surgery (Table); however, it can also present as a progression of myasthenia gravis. Patients should be monitored in the intensive care unit with respiratory status checks every 2-4 hours using vital capacity (VC) and maximal inspiratory force (MIF). Both VC and MIF should be interpreted in combination as neither is superior to the other. Patients require intubation for VC <20 mL/kg or MIF >-30 cm H2O (eg, 0 to -30).
Anticholinesterase inhibitors should be stopped temporarily while the patient is on mechanical ventilation to minimize secretions. Rapid treatment involves plasmapheresis or intravenous immunoglobulin (IVIG) in addition to high-dose glucocorticoids (prednisone 60-80 mg/day) due to the short-lived therapeutic effect of plasmapheresis and IVIG. Patients who cannot tolerate glucocorticoids can be started on azathioprine, mycophenolate mofetil, or cyclosporine. Weaning and extubation are considered in patients with improved muscle strength (eg, ability to lift head off bed, VC >20 mL/kg, MIF <-30 cm H2O).
(Choices A, C, D, and E) Arterial PCO2, oxygen saturation, peak expiratory flow rate, and respiratory rate are not good predictors of impending respiratory failure as they may not show marked abnormalities until late stages.