movement disorders
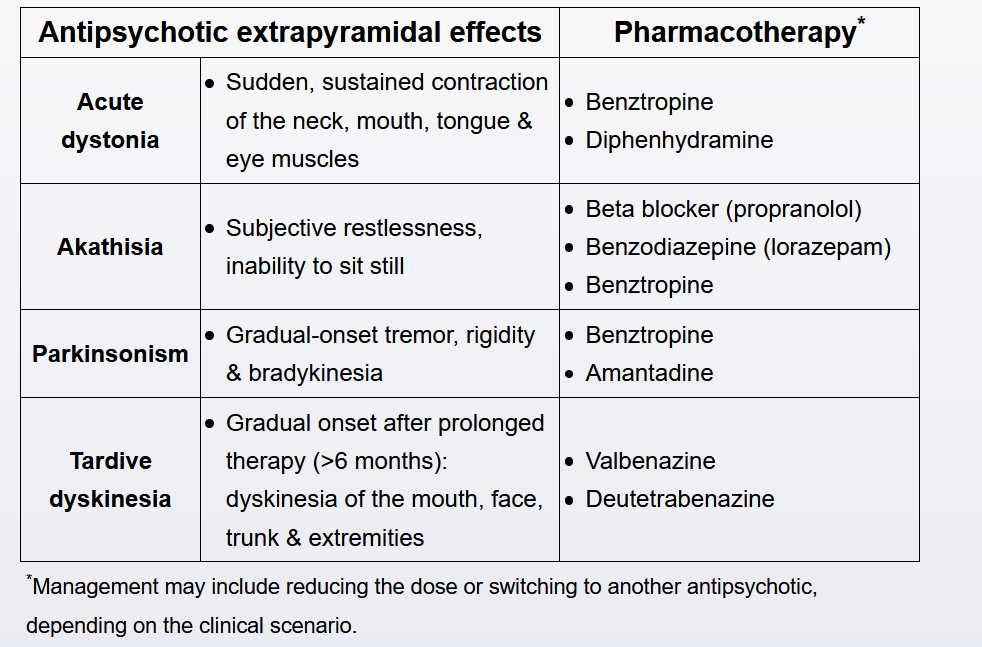
This patient is experiencing an acute dystonic reaction manifested by torticollis and an oculogyric crisis (forced, sustained elevation of the eyes in an upward position). Acute dystonia is a type of extrapyramidal symptom (EPS) that develops within hours to days of starting or dose escalation of antipsychotics. This patient's risk factors include young age, male sex, and use of a high-potency, first-generation antipsychotic (haloperidol). Other types of EPS include akathisia (inner restlessness) and drug-induced parkinsonism (tremor, rigidity, bradykinesia, masked facies).
PD
Parkinson disease (PD) is a clinical diagnosis that requires the presence of bradykinesia in addition to either tremor or rigidity. The majority of patients will have all of these physical findings at some point in their disease course. A clear response to dopaminergic therapy (eg, levodopa/carbidopa, pramipexole) is also highly supportive of the diagnosis. Other features suggestive of the disease include a unilateral onset and persistent asymmetry of symptoms. Asymmetric hand rigidity would be the finding most consistent with the diagnosis of PD in this patient.
Parkinson-plus syndromes (eg, progressive supranuclear palsy, multiple system atrophy) can also present with bradykinesia and rigidity; however, distinguishing features include rapid progression, symmetric motor signs, lack of tremor, falls early in the course of the disease, dysautonomia, and a poor response to dopaminergic therapy.
Gaze palsy is more consistent with progressive supranuclear palsy (PSP), a Parkinsonian-plus syndrome characterized by problems with vertical gaze and falls due to postural instability. Resting tremor is rare in PSP.