mixed cryoglobulinemia
- related: hepatitis
- tag: #GI, #dermatology
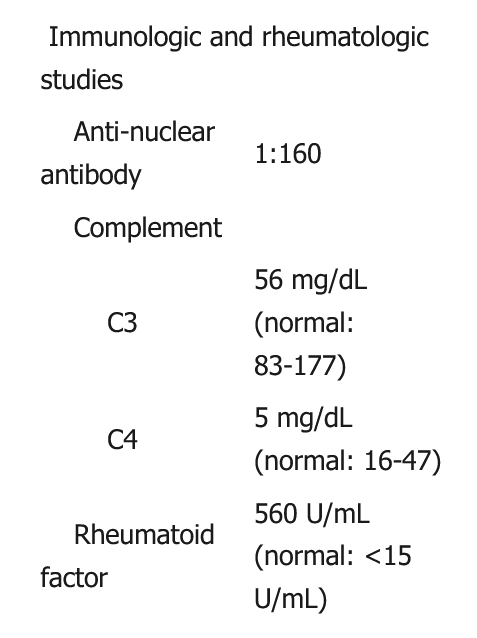
This patient has renal insufficiency with palpable purpura, elevated rheumatoid factor, and hypocomplementemia, raising suspicion for mixed cryoglobulinemia syndrome. The diagnosis can be confirmed by measuring serum cryoglobulin levels.
Mixed cryoglobulinemia syndrome is a vasculitis due to the deposition of immune complexes (polyclonal IgG and IgM rheumatoid factor) within the vascular wall of small- and medium-size vessels. Most cases arise in those with chronic HCV virus (as is likely in this patient with a history of intravenous drug use), but patients with lymphoproliferative disorders, autoimmune disease, and other infections are also at risk.
Patients with mixed cryoglobulinemia syndrome most commonly develop a triad of manifestations:
- Palpable purpura: the vasculitis may manifest as skin ulceration and necrosis.
- Weakness
- Arthralgias

Other nonspecific symptoms (eg, nausea) and peripheral neuropathy also frequently occur. Laboratory examination typically reveals elevated rheumatoid factor and hypocomplementemia. Approximately 20% of patients develop glomerulonephritis (red cells, red cell casts, proteinuria) with or without renal insufficiency.
Most cases of mixed cryoglobulinemia syndrome are secondary to an underlying inflammatory condition, which generates the immune complexes that drives the vasculitis. As such, the treatment of mixed cryoglobulinemia syndrome is typically divided into 2 stages:
- Initial immunosuppressive therapy – stabilizes end-organ damage (eg, glomerulonephritis) using rituximab plus prednisone
- Treatment of underlying disease – targeted therapy against the condition that triggered the cryoglobulinemia
This patient received initial immunosuppressive therapy, and his renal function stabilized. He now requires treatment of the underlying condition that triggered the cryoglobulinemia. The most likely causative factor in this patient with intravenous drug use, hepatomegaly, and elevated aminotransferases is chronic hepatitis C virus. Treatment with antiviral therapy will likely be required.