minimal change glomerulopathy
- related: Nephrology
- tags: #note
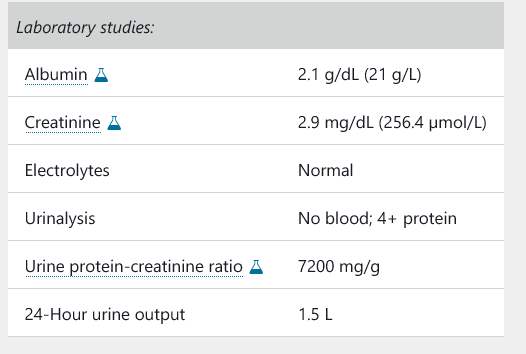
An 81-year-old man is hospitalized for an acute onset of edema in his legs and abdomen. History is significant for chronic back pain, for which he takes daily ibuprofen. He has no other symptoms.
On physical examination, vital signs are normal. There is no rash. Cardiac examination is without extra sounds or murmurs, and the estimated central venous pressure is normal. The lungs are clear on examination. Ascites is noted. There is 3-mm pitting edema of the extremities to the mid thigh.
Doppler ultrasound of the kidneys is unremarkable.
A kidney biopsy is the most appropriate next step for this patient who has the nephrotic syndrome most likely caused by minimal change glomerulopathy (MCG). MCG is the cause of the nephrotic syndrome in 10% to 15% of adults, with a significantly higher incidence in elderly patients (≥65 years of age) and very elderly patients (≥80 years of age). Most cases are idiopathic, but secondary causes must be considered in adults, including medications such as NSAIDs. Adults with MCG present with acute kidney injury (AKI) in up to 25% of cases. Factors associated with AKI include older age, male sex, hypertension, low serum albumin levels, and heavier proteinuria. The differential diagnosis for the nephrotic syndrome with AKI is limited to only a few entities: MCG with acute tubular necrosis or allergic interstitial nephritis, membranous glomerulopathy with bilateral renal vein thrombosis, amyloidosis with cast nephropathy, and collapsing focal segmental glomerulosclerosis. A kidney biopsy is therefore required to make the correct diagnosis.
Although this presentation is most suggestive of MCG given the patient's age, empiric glucocorticoids would not be indicated without a biopsy-confirmed diagnosis because glucocorticoid monotherapy would not be efficacious in the treatment of membranous glomerulopathy or amyloidosis.
Treatment
Diuretics plus high-dose prednisone is the most appropriate treatment for this patient with minimal change glomerulopathy (MCG; also known as minimal change disease). MCG is the most common cause of the nephrotic syndrome in children and accounts for approximately 10% to 15% of cases in adults. Immunosuppressive therapy is indicated for treatment of primary MCG, which invariably presents with the full nephrotic syndrome. The concomitant acute tubular necrosis makes treatment even more imperative in this case, because primary MCG with acute kidney injury has been shown to be a treatment-responsive lesion if treated in a timely manner. First-line therapy is prednisone at a dose of 1 mg/kg per day or 2 mg/kg every other day for 8 to 12 weeks, followed by a taper. Patients typically respond to glucocorticoids within 8 to 16 weeks. However, relapse is common, and in a substantial percentage of patients, the course of MCG is one of remission followed by relapse. For frequently relapsing or glucocorticoid-dependent disease, treatment options include cyclophosphamide, calcineurin inhibitors (tacrolimus or cyclosporine), mycophenolate mofetil, and rituximab. In addition to immunosuppression, patients should receive standard therapy for the nephrotic syndrome, including an ACE inhibitor or angiotensin receptor blocker (this patient is already taking lisinopril, with well-controlled blood pressure), diuretics for edema management, and cholesterol-lowering medication if total cholesterol >200 mg/dL (5.1 mmol/L). In rare cases of MCG secondary to malignancies (Hodgkin lymphoma, non-Hodgkin lymphoma, thymoma), medications (NSAIDs, lithium), infections (strongyloides, syphilis, mycoplasma, ehrlichiosis), and atopy (pollen, dairy products), treatment of the underlying condition without immunosuppression may be sufficient.