meningitis
- related: neisseria meningitis, cryptococcus, TB meningitis, lumbar puncture
Treatment
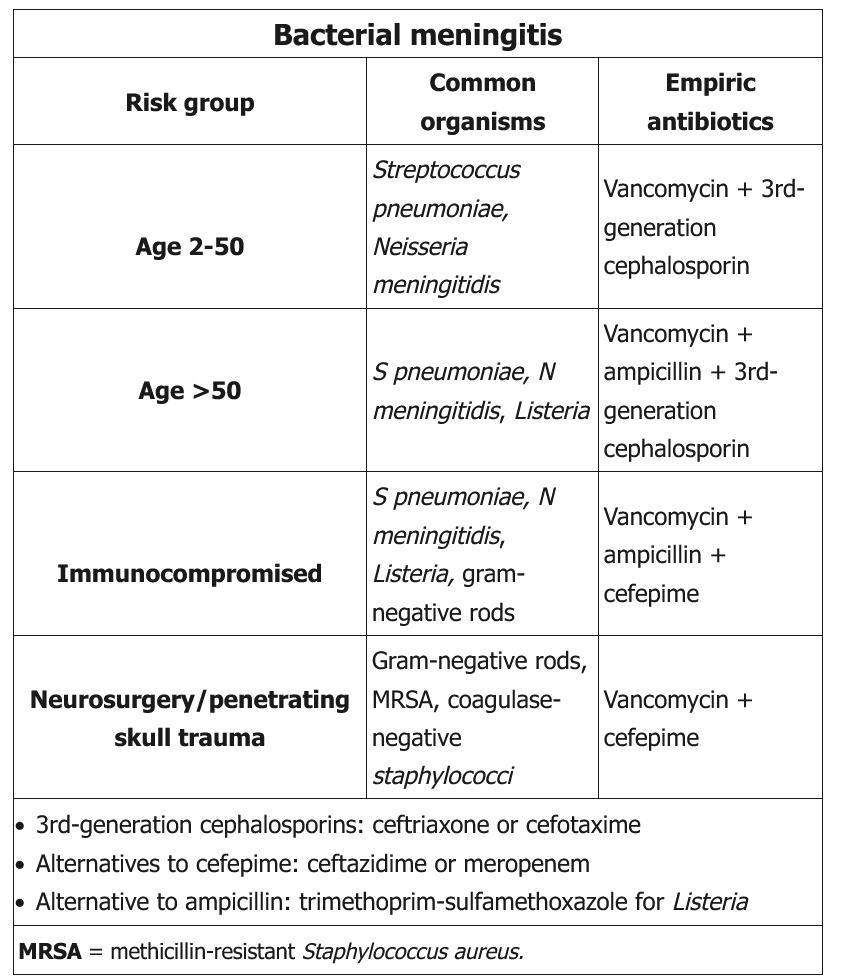
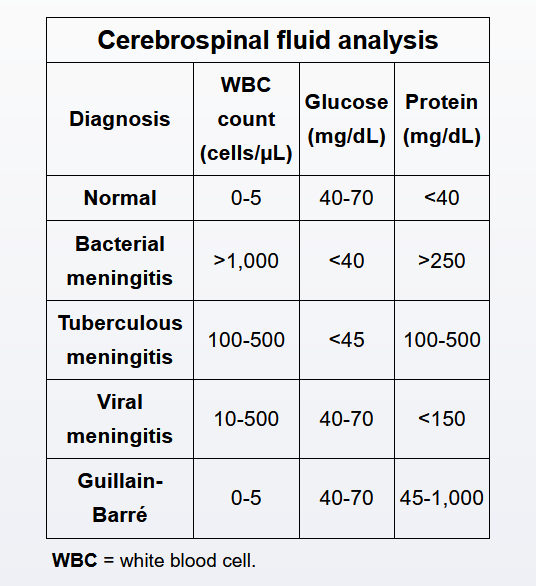
This patient presents with acute hospital-acquired (healthcare-associated) bacterial meningitis after recent brain surgery. The lumbar puncture findings of neutrophilic pleocytosis, elevated protein, and low CSF glucose strongly suggest a bacterial etiology. Following brain surgery, the most likely organisms to cause meningitis include gram-negative bacilli (e.g., Pseudomonas aeruginosa) and gram-positive cocci (e.g., methicillin resistant Staphylococcus aureus). Both cefepime and ceftazidime have good CNS penetration as well as broad coverage against gram-negative organisms, especially Pseudomonas aeruginosa, and some coverage against gram-positive organisms (e.g., Streptococcus pneumoniae). Vancomycin is effective against MRSA.
Ceftriaxone and vancomycin are appropriate for empiric treatment of community-acquired meningitis in patients aged 2-50 years, as this combination retains good coverage against S. pneumoniae. However, ceftriaxone does not adequately cover Pseudomonas. Acyclovir is not needed as HSV meningitis is unlikely.
Piperacillin/tazobactam has good coverage against Pseudomonas and other gram-negative organisms, but does not have good CNS penetration.
Ampicillin is usually added in suspected bacterial meningitis to cover for Listeria monocytogenes in patients > age 50 or the immunocompromised.