lower GI bleed
- related: GI
Resuscitation goals for patients with LGIB should be normalization of blood pressure and heart rate, as well as the transfusion of packed red blood cells if needed to maintain the hemoglobin level above 7 g/dL (70 g/L), with a threshold of 9 g/dL (90 g/L) in patients with massive bleeding, or when treatment may be delayed. Platelet transfusion to maintain counts above 50,000 cells/µL (50 × 109/L) is recommended in patients with active bleeding.
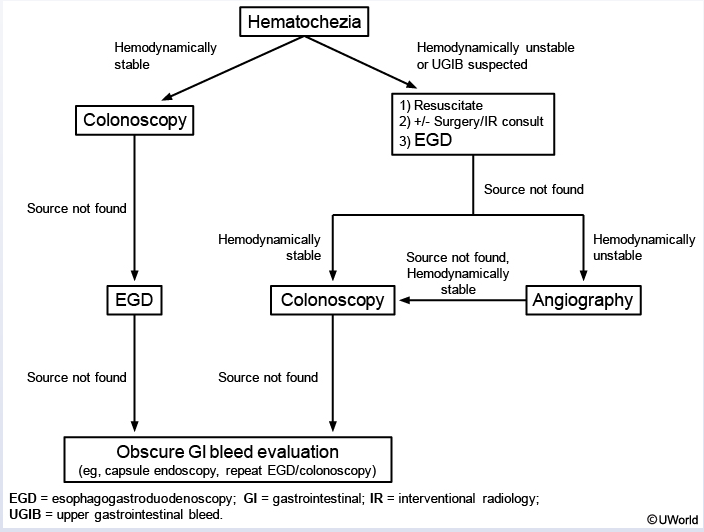
CT angiography (CTA) is the initial diagnostic test in patients who are hemodynamically unstable or have rapid ongoing bleeding. Upper endoscopy may be a reasonable first choice in patients at risk for a rapidly bleeding upper gastrointestinal source as a cause of hematochezia. If CTA does not show a source of bleeding in the unstable or rapidly bleeding patient, upper endoscopy should be performed immediately.
Among hemodynamically stable patients without evidence of rapid bleeding, colonoscopy is the first test of choice in patients with LGIB. It should be performed within 24 hours of presentation after adequate colon preparation in patients with significant bleeding. Colonoscopy identifies a source of LGIB in two thirds of patients.
Radiographic studies should be considered in patients with ongoing bleeding who do not respond to resuscitation, patients who cannot tolerate colonoscopy or colon preparation, or patients in whom a source of bleeding is not identified endoscopically. Techniques include CT angiography, angiography, and, less frequently, tagged red blood cell scintigraphy.
Catheter-based angiography with embolization should be performed as soon as possible if CTA shows active bleeding. Angiographic embolization is also frequently used to stop persistent or recurrent diverticular bleeding because endoscopic approaches are limited due to the typical location of the vessel inside a thin-walled diverticulum. Surgical consultation is usually reserved for patients who do not respond to endoscopic or radiographic measures.
The risk for rebleeding is highest in patients with diverticular bleeding (9% to 47%) and angiodysplasia bleeding (37% to 64%). For prevention of recurrent LGIB, nonaspirin NSAIDs should be avoided, particularly after diverticular or angiodysplasia bleeding. Decisions on continued use of antiplatelet or anticoagulants and timing of resuming therapy must balance the likelihood of rebleeding and thrombotic risk. Aspirin for primary prevention of cardiovascular disease should be discontinued and not restarted. In patients with high-risk cardiovascular disease, aspirin for secondary prevention should be discontinued only if necessary and be restarted as soon as possible after hemostasis is achieved. Decisions about discontinuation of dual antiplatelet therapy with a P2Y12 receptor antagonist and aspirin in patients with a recent acute coronary syndrome or coronary stent placement should be made in conjunction with a cardiologist. In patients with significant hemorrhage in whom a P2Y12 receptor antagonist must be discontinued, aspirin should be continued and the P2Y12 receptor antagonist restarted within 5 days.
In patients receiving warfarin who have hemodynamically significant hemorrhage, warfarin should be discontinued and reversed with prothrombin complex concentrate and vitamin K. Re-anticoagulation with low-molecular-weight heparin or unfractionated heparin should be considered within 48 hours in patients at high thrombotic risk (that is, those with a mechanical prosthetic heart valve in mitral position, atrial fibrillation with prosthetic heart valve or mitral stenosis, or recent venous thromboembolism). In patients receiving non–vitamin K antagonist oral anticoagulants, the anticoagulant should be discontinued on presentation, and, if significant hemorrhage is present, reversal with the appropriate reversal agent (idarucizumab or andexanet) should be considered. The timing of resuming therapy with non–vitamin K antagonist oral anticoagulants depends on the risk profile, but generally resumption should occur within 7 days.