legionella pneumonia
- related: Pulmonology, Pneumonia
- tags: #pulmonology
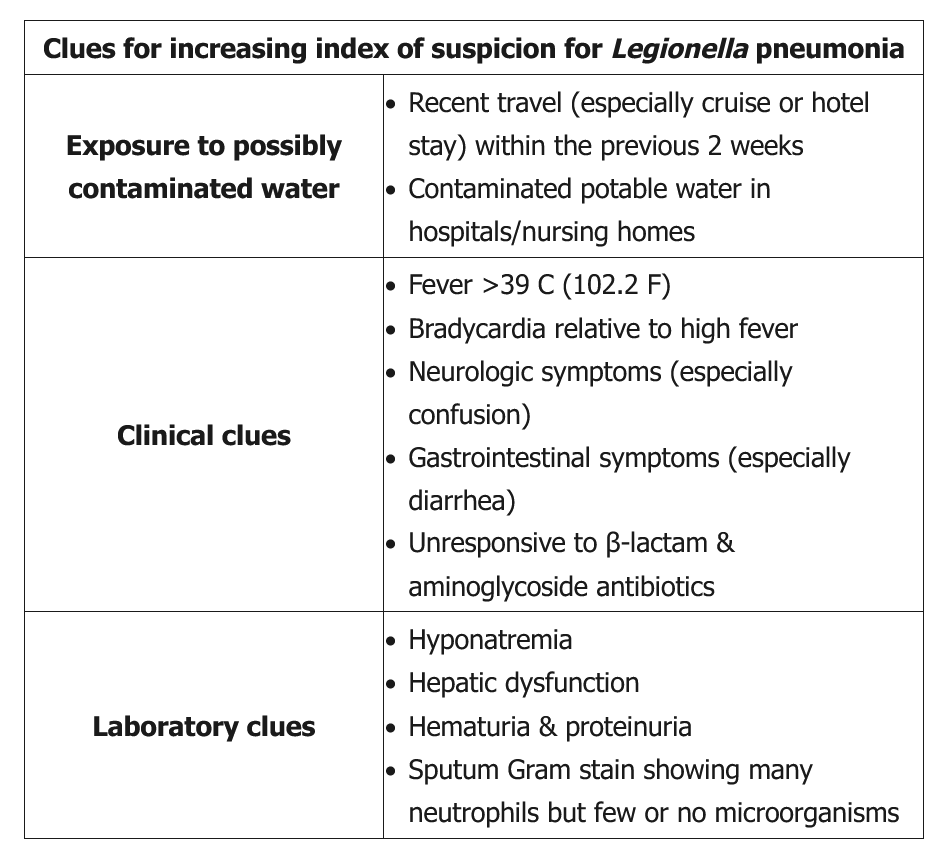
This patient’s underlying risk factors (elderly age, COPD, nursing home resident), clinical presentation (confusion, high fever with bradycardia), laboratory abnormalities (hyponatremia, thrombocytopenia, elevated LFTs), and failure to respond to vancomycin and piperacillin-tazobactam are strongly suggestive of Legionella pneumonia. Legionella species are facultative intracellular gram-negative bacilli whose natural habitats are aquatic bodies (e.g., lakes, streams, man-made reservoirs, standing water).
There are no pathognomonic or highly specific clinical, laboratory, or radiological features for Legionella infection. The most common x-ray finding is a unilobar infiltrate that progresses to consolidation. Patients with suspected Legionella pneumonia should have both a urinary Legionella antigen test (detects only L. pneumophila, serogroup 1) and a respiratory sample (e.g., sputum, BAL) for Legionella culture. Suspected or proven Legionella pneumonia requires treatment with a respiratory fluoroquinolone (e.g., levofloxacin) or “newer” macrolide (e.g., azithromycin), as both have good lung penetration with potent intracellular activity.
Ampicillin and piperacillin-tazobactam are both beta-lactam antibiotics and are ineffective against Legionella. Ampicillin is commonly used to treat Listeria, which causes meningitis/sepsis but not pneumonia.
Linezolid is approved for treating MRSA pneumonia and is as effective as vancomycin. However, vancomycin and linezolid are not effective against Legionella.
Metronidazole is effective for anaerobic aspiration pneumonia but not for Legionella.