juvenile idiopathic arthritis
- related: pediatric
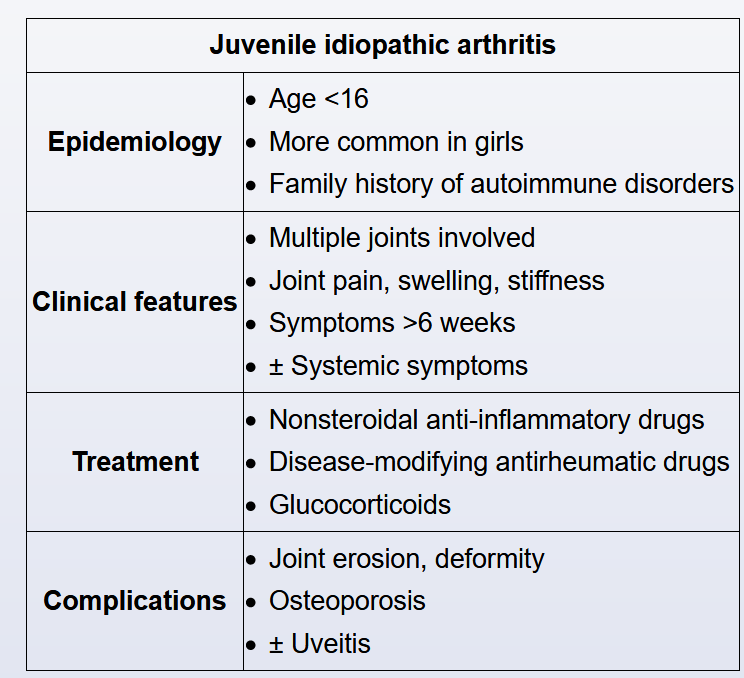
This patient with midline spinal point tenderness most likely has a vertebral compression fracture due to poorly controlled juvenile idiopathic arthritis (JIA)-associated osteoporosis. JIA is a chronic (>6 weeks), relapsing-remitting inflammatory condition that causes pain, swelling, and stiffness of multiple joints. The disease varies in severity and may be difficult to control. Treatment includes a combination of nonsteroidal anti-inflammatory drugs (eg, naproxen), disease-modifying antirheumatic drugs (eg, methotrexate), and glucocorticoids.
Prolonged glucocorticoid use is generally avoided due to side effects. However, patients with refractory JIA may require short courses of low-dose systemic glucocorticoids to treat flares. The combination of frequent systemic glucocorticoid use and continued joint destruction from unremitting disease may result in decreased bone mineral density (ie, osteoporosis).
Low bone mass associated with osteoporosis increases the risk for fractures. Any pressure (eg, coughing, bending) or minor trauma can result in a pathologic fracture, and vertebral compression fractures are among the most common. Localized back pain that worsens with movement is typical for these fractures, as seen in this patient. Dual-energy x-ray absorptiometry is used to diagnose osteoporosis and predict fracture risk. Supplemental calcium and vitamin D are recommended to optimize bone health.