interstitial cystitis
- related: UTI, Nephrology
- tags: #nephrology
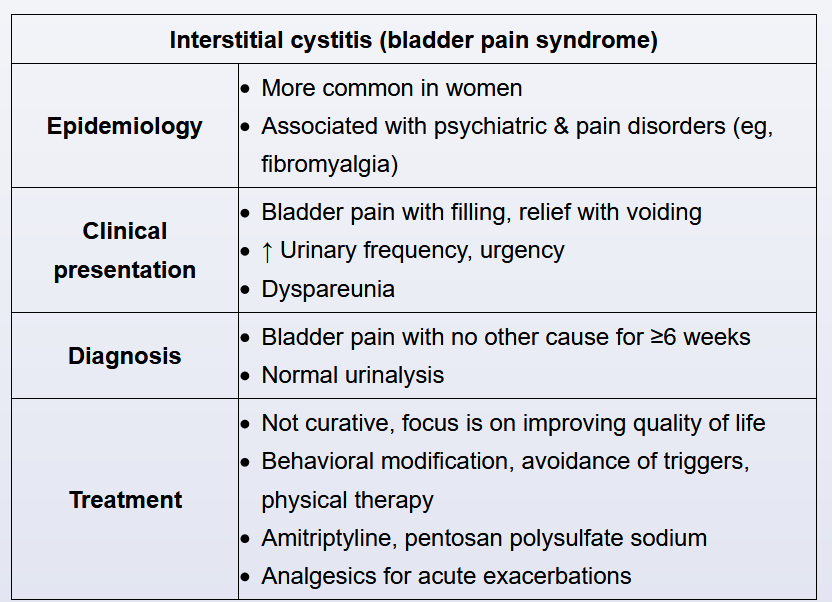
Interstitial cystitis (also known as painful bladder syndrome) is a chronic, painful bladder condition of uncertain etiology. The pelvic pain in interstitial cystitis is classically exacerbated by bladder filling and relieved by voiding. The onset of the symptoms is typically gradual, and the symptoms worsen over a period of months. Other characteristic symptoms include urinary urgency and frequency, and chronic pelvic pain. Other presenting symptoms include urinary urgency, nocturia, and frequency. Patients often deliberatively urinate frequently to prevent the bladder from being full. The pain can be exacerbated by exercise, sexual intercourse (dyspareunia), and alcohol consumption.
The diagnosis of interstitial cystitis is primarily clinical. Urinalysis is obtained to exclude other causes of bladder pain (eg, urinary tract infection, sexually transmitted disease, cancer); results are normal in interstitial cystitis. Treatment is palliative and includes trigger avoidance, amitriptyline, and analgesics for pain flares.
Treatment of IC/BPS is not curative and, therefore, focuses on patient education, quality of life, and avoidance of triggers. Some oral pharmacotherapies improve symptoms; the most common treatments include amitriptyline and pentosan polysulfate sodium. Amitriptyline, a tricyclic anticholinergic, relieves bladder pain and associated depressive symptoms; however, side effects (eg, dry mouth, orthostatic hypotension) limit its use. Pentosan polysulfate sodium repairs the urothelium, has minimal side effects (eg, mild reversible hair loss), and is approved by the FDA for the treatment of IC/BPS. Bladder instillation therapy (eg, hydrodistension), intradetrusor botulinum toxin, and sacral neuromodulation are reserved for severe or refractory cases.