infant disorders
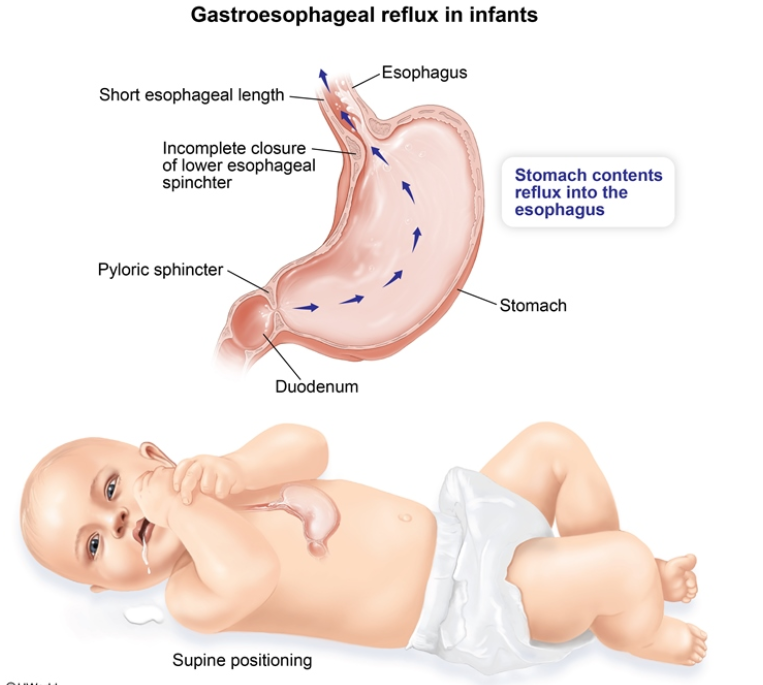
Gastroesophageal reflux (GER), or spit-up, is common and normal in the majority of infants as they have a relatively relaxed lower esophageal sphincter. The esophagus is also shorter and the stomach is smaller compared with that of older children. Breastmilk and formula are easily regurgitated up the esophagus and out of the mouth; however, the episodes do not cause injury, weight loss, or other complications. Infants are commonly described as "happy spitters," and GER is colloquially referred to as "a laundry problem, not a medical problem."
GER is distinguished clinically from gastroesophageal reflux disease (GERD), which causes complications such as weight loss, feeding refusal, respiratory complications (eg, aspiration), and significant pain with back-arching and irritability during feeds.
This patient has appropriate weight gain and no pain with feeds, which is consistent with physiologic GER. Initial management includes reassurance and lifestyle modifications. Upright positioning after feeds, burping during feeds, and frequent, small-volume feeds are first-line interventions. GER is typically more frequent during the first few months of life, with peak symptoms around age 4 months; it is expected to self-resolve by age 12-18 months.
IDA
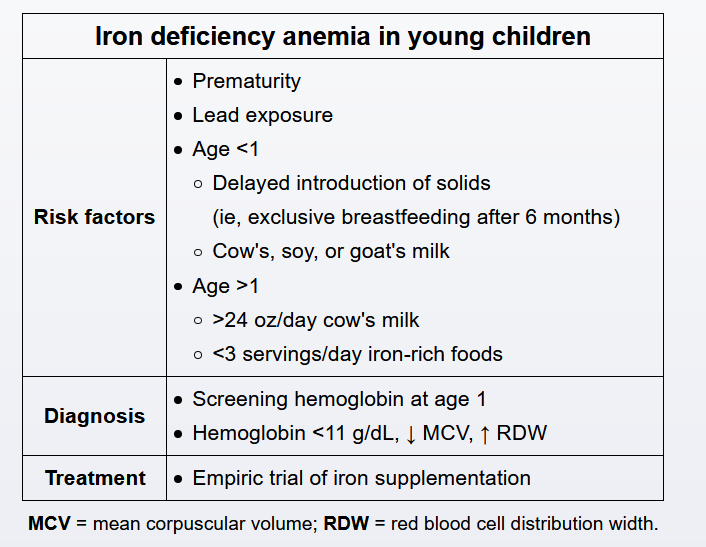
Iron deficiency is the most common nutritional deficiency in children and should be suspected in any child drinking >24 oz of cow's milk per day. Fatigue and pallor may occur, but patients are often asymptomatic and detected on universal screen around age 1. Given the high prevalence of iron deficiency anemia in infants and toddlers, a presumptive diagnosis of iron deficiency is made when hemoglobin <11 g/dL. Lead level should also be measured, but additional studies are usually not needed in the initial workup. An empiric trial of ferrous sulfate is considered the most cost-effective treatment, and the doses should be given with juice between meals as vitamin C facilitates iron absorption. Patients should also be advised to limit milk intake to <20 oz per day and to increase intake of iron-rich foods (eg, meats, fortified cereals).
Diabetic infant
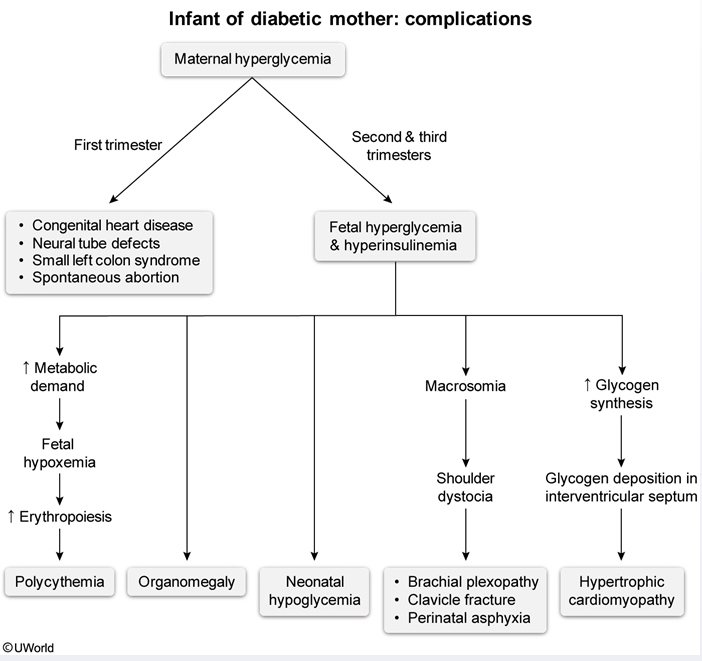
This newborn with respiratory distress (tachypnea, nasal flaring, retractions) and a heart murmur likely has transient hypertrophic cardiomyopathy, a cardiac anomaly found in infants of mothers with gestational diabetes. This disease occurs in the late second to early third trimesters due to fetal hyperinsulinemia in response to maternal and fetal hyperglycemia. Insulin triggers glycogen synthesis, and excess glycogen and fat are deposited within the myocardium, particularly the interventricular septum. Increased oxidative stress of the interventricular septum may contribute to this selective thickening.
A hypertrophic interventricular septum is usually asymptomatic; however, if left ventricular outflow is obstructed, manifestations of congestive heart failure may occur. In infants, these can include respiratory distress, tachycardia, and hypoxia (as seen in this patient), as well as failure to thrive. Despite the presence of pulmonary edema, crackles may not be auscultated. Pulmonary congestion and cardiomegaly may be evident on chest radiograph, and echocardiography confirms the diagnosis. Although transient tachypnea of the newborn is a common cause of tachypnea and respiratory distress, this patient's murmur makes cardiogenic pulmonary edema due to transient hypertrophic cardiomyopathy the most likely etiology.
Poorly controlled gestational diabetes mellitus carries numerous additional risks for the infant, including macrosomia, hypocalcemia, hypoglycemia, hyperviscosity due to polycythemia, and respiratory difficulties. Most of these adverse effects can be avoided with strict glycemic control throughout pregnancy (ideal fasting blood glucose ≤95 mg/dL).
Hypoplastic left ventricle (ie, hypoplastic left heart syndrome) is an embryologic malformation that occurs early in the first trimester in infants of mothers with pregestational diabetes. It presents with cyanosis, and the structural abnormality is often recognized on second-trimester ultrasound.