inappropriately normal TSH could be sign of central hypothyroidism
- related: Endocrine, hypothyroidism
- tags: #endocrine
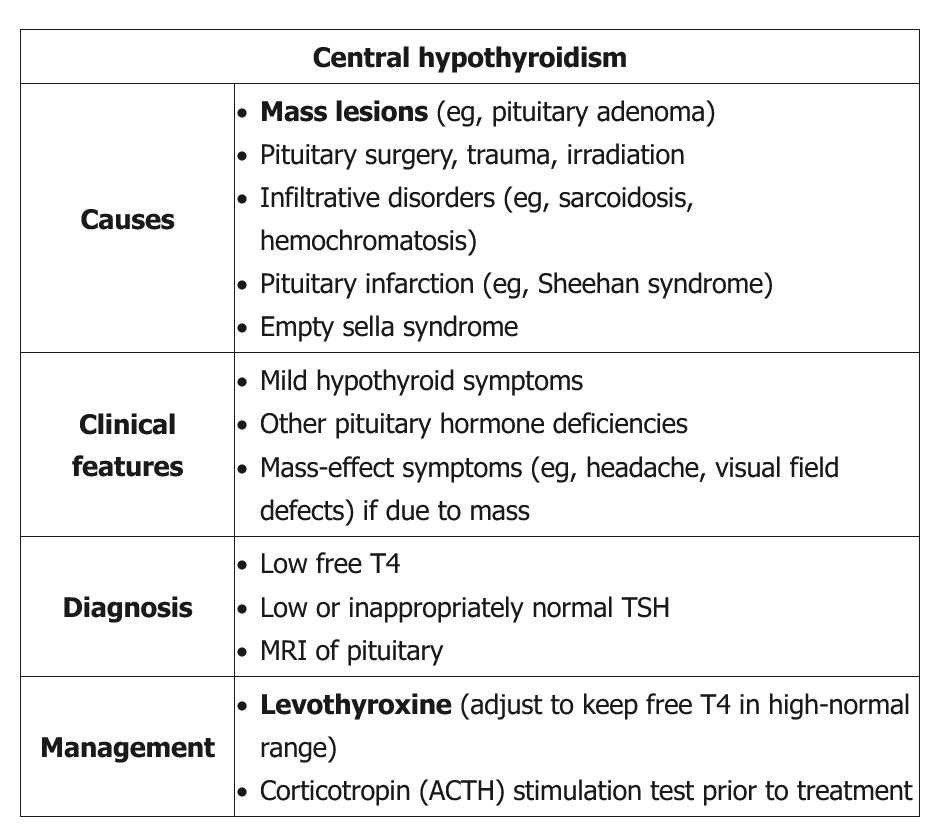
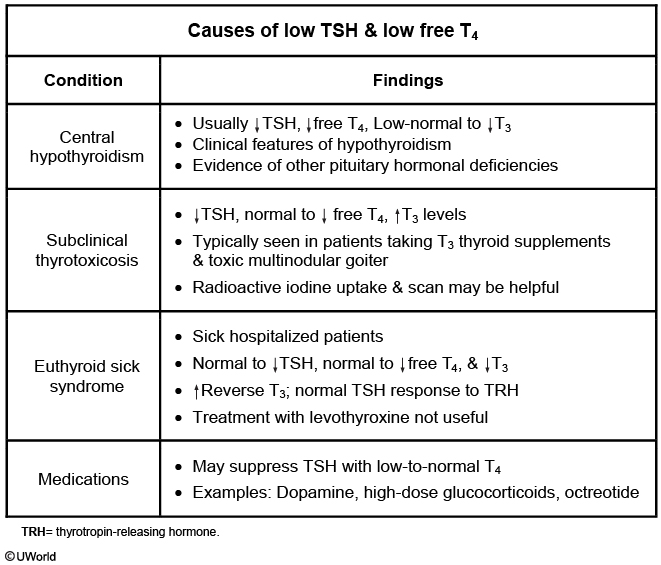
This patient's clinical findings (eg, fatigue, weight gain, dry skin, hyponatremia, normocytic anemia) are suggestive of hypothyroidism, but his TSH is not elevated. In light of his history of pituitary radiation, this presentation likely represents central hypothyroidism. In primary hypothyroidism TSH is usually elevated, but in central hypothyroidism TSH is typically low or inappropriately normal (although it may occasionally be mildly high in patients who secrete biologically inactive TSH) (caused by failure of pituitary to regulate TSH). A low serum free T4 can confirm the diagnosis of central hypothyroidism.
Pituitary masses are the most common cause of central hypothyroidism, due to direct compression by the tumor or late effects of surgery or radiation therapy. If the cause is not known, patients should undergo MRI of the pituitary to rule out a mass lesion. Patients with central hypothyroidism should also be tested for abnormalities of other pituitary hormones (eg, ACTH, growth hormone, gonadotropins). The treatment is levothyroxine with the dose adjusted to maintain free T4 in the high-normal range. Unlike in primary hypothyroidism, TSH is not used to monitor therapy as it will remain low.
All patients with central hypothyroidism should undergo neuroimaging to evaluate for pituitary/hypothalamic masses and chemical testing for pituitary hormones (especially adrenal). Glucocorticoid deficiency must be diagnosed and treated in patients with central hypothyroidism before starting levothyroxine therapy. Patients with undiagnosed and untreated secondary insufficiency who are given levothyroxine can develop adrenal crisis. Levothyroxine dosing is adjusted to the patient's symptoms and/or maintaining free T4 levels at the upper part of normal range. Other hormone deficiencies should also be concurrently treated.