Hypercalcemia
- related: Endocrine, hypocalcemia
- tags: #note
Symptoms
- confusion
- delirium
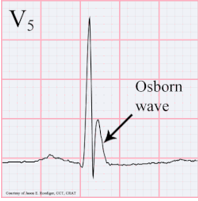
- short QT
This patient has newly discovered hypercalcemia. Patients with mild hypercalcemia are often asymptomatic, but common initial manifestations may include constipation (as in this patient), fatigue, nausea, and nephrolithiasis.
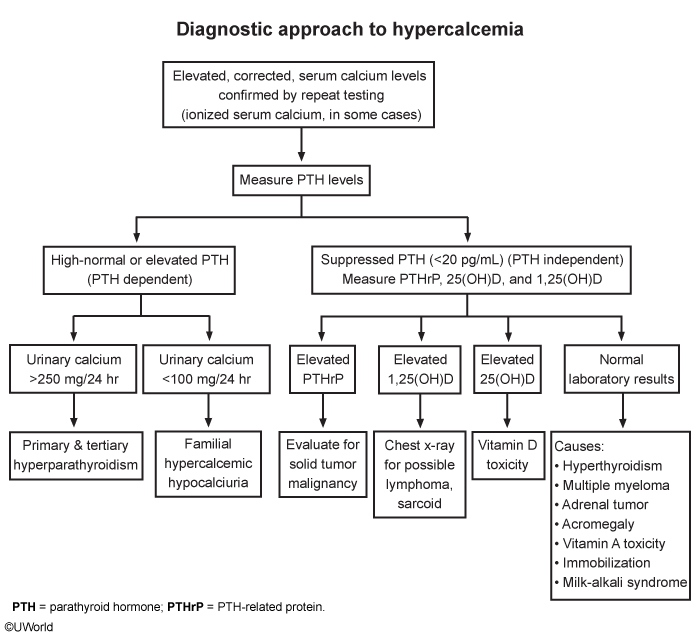
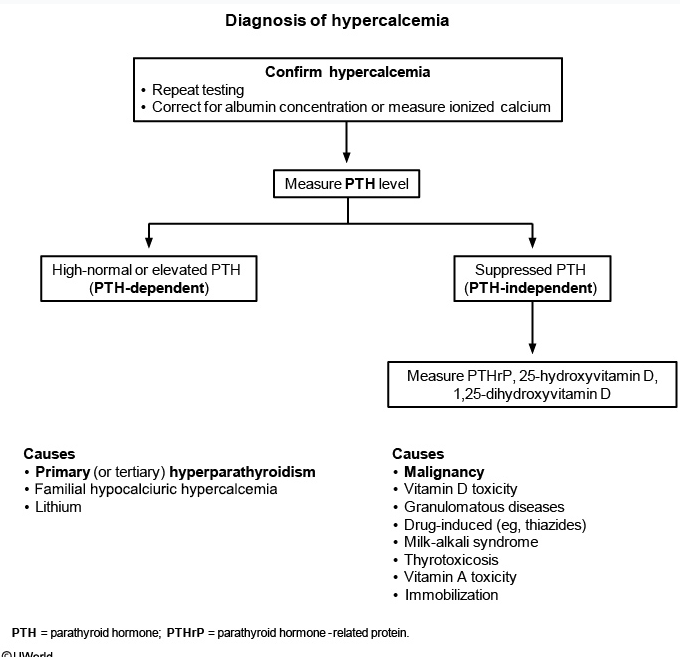
The first step in the evaluation of hypercalcemia is to repeat the serum calcium with concurrent measurement of serum parathyroid hormone (PTH) to distinguish PTH-dependent (eg, primary hyperparathyroidism) from non-PTH-dependent causes. Hypercalcemia with an elevated (or high-normal) PTH suggests excessive secretion of PTH, whereas non-PTH-dependent causes have suppressed PTH secretion (PTH <20 pg/mL).
Even when malignancy is suspected, PTH remains the first step in the evaluation of hypercalcemia as the incidence of primary hyperparathyroidism is higher in patients with cancer than in the general population. Assay results are generally available within a few hours.
Subsequent testing in patients with non-PTH-dependent hypercalcemia may include chest x-ray (eg, for malignancy, granulomatous diseases), serum and urinary protein electrophoresis (for multiple myeloma), PTH-related protein (for humoral hypercalcemia of malignancy), and vitamin D levels (eg, for exogenous vitamin D intake, granulomatous diseases). However, PTH should be measured first to rule out hyperparathyroidism, especially in a stable outpatient.
Urinary calcium should be measured in patients with PTH-dependent hypercalcemia to differentiate familial hypocalciuric hypercalcemia (a rare disorder due to mutations in the calcium-sensing receptor and leading to low urinary calcium excretion) from primary hyperparathyroidism (in which urinary calcium excretion is normal or elevated), but only after PTH-dependent hypercalcemia is confirmed.
Squamous cell carcinoma is associated with elevated PTHrP causing hypercalcemia. However, it does not usually cause elevated 1,25-hydroxy vitamin D.
Thyrotoxicosis can also result in hypercalcemia but does not usually cause elevated 1,25-hydroxy vitamin D.
Vitamin D intoxication increases calcium and bone resorption causing hypercalcemia, but usually occurs at 25-hydroxy vitamin D levels > 150 ng/mL. Vitamin D intoxication does not cause elevated 1,25-hydroxy vitamin D. Given this patient’s hilar adenopathy, sarcoidosis or lymphoma is more likely.
Parathyroid adenoma usually presents with elevated or high-normal PTH out of proportion to the hypercalcemia. However, this patient’s low-normal PTH makes this unlikely.
Patients with suppressed PTH should have measurement of PTH-related peptide (PTHrP) and both 1,25-hydroxy vitamin D and 25-hydroxy vitamin D. Elevated PTHrP usually indicates solid tumor malignancy, while elevated 25-hydroxy vitamin D indicates vitamin D toxicity. This patient has elevated 1,25-hydroxy vitamin D, which is usually seen in granulomatous diseases and lymphoma. Sarcoidosis is a multisystem granulomatous disease with noncaseating tissue granulomas. Activated pulmonary macrophages produce calcitriol, which is responsible for the hypercalcemia and hypercalciuria.
Cancer
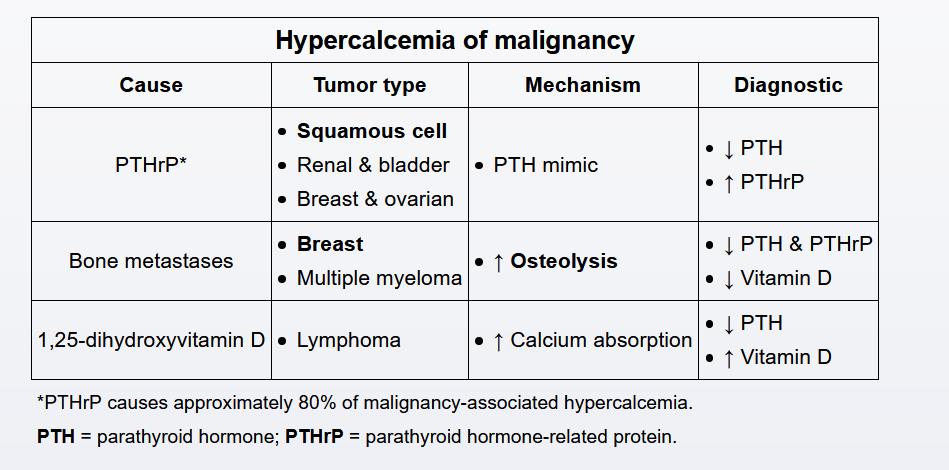
The most common cause of non-parathyroid hormone (PTH)-dependent hypercalcemia is humoral hypercalcemia of malignancy (HHM), which is due to secretion of PTH-related protein (similar to PTH and binds PTH receptors). Hypercalcemia in primary hyperparathyroidism is usually mild (calcium <12 mg/dL) and often asymptomatic, whereas HHM is typically more acute and severe. Renal dysfunction may occur due to dehydration from polyuria and vomiting, and hypercalcemia-induced vasoconstriction of intrarenal blood vessels. Other causes of cancer-associated hypercalcemia include overproduction of 1,25-dihydroxyvitamin D (eg, certain lymphomas) and bony metastases (eg, multiple myeloma).
This patient has severe hypercalcemia with suppressed PTH (<20 pg/mL), which, in light of his smoking history and associated weight loss, most likely represents HHM due to squamous cell carcinoma of the lung. Although HHM is most often seen in patients with known malignancy, hypercalcemia may occasionally be the presenting feature. HHM is typically seen in advanced malignancy and confers a poor prognosis.
Treatment
short term
- IV fluids
- Can add Lasix if have heart failure, renal failure, or volume overload
- Calcitonin: can use acutely to decrease Ca.
- Use if EKG changes, renal failure, AMS
- Exhibits tachyphylaxis, less effective over time
Long term
- Bisphosphonate: zoledronic acids
- antiresorptive used in osteoporosis
- inhibits osteoclasts
- takes days to work
- don't use until have diagnosis or plan
Dialysis
- severe renal failure