histoplasmosis
- related: ID
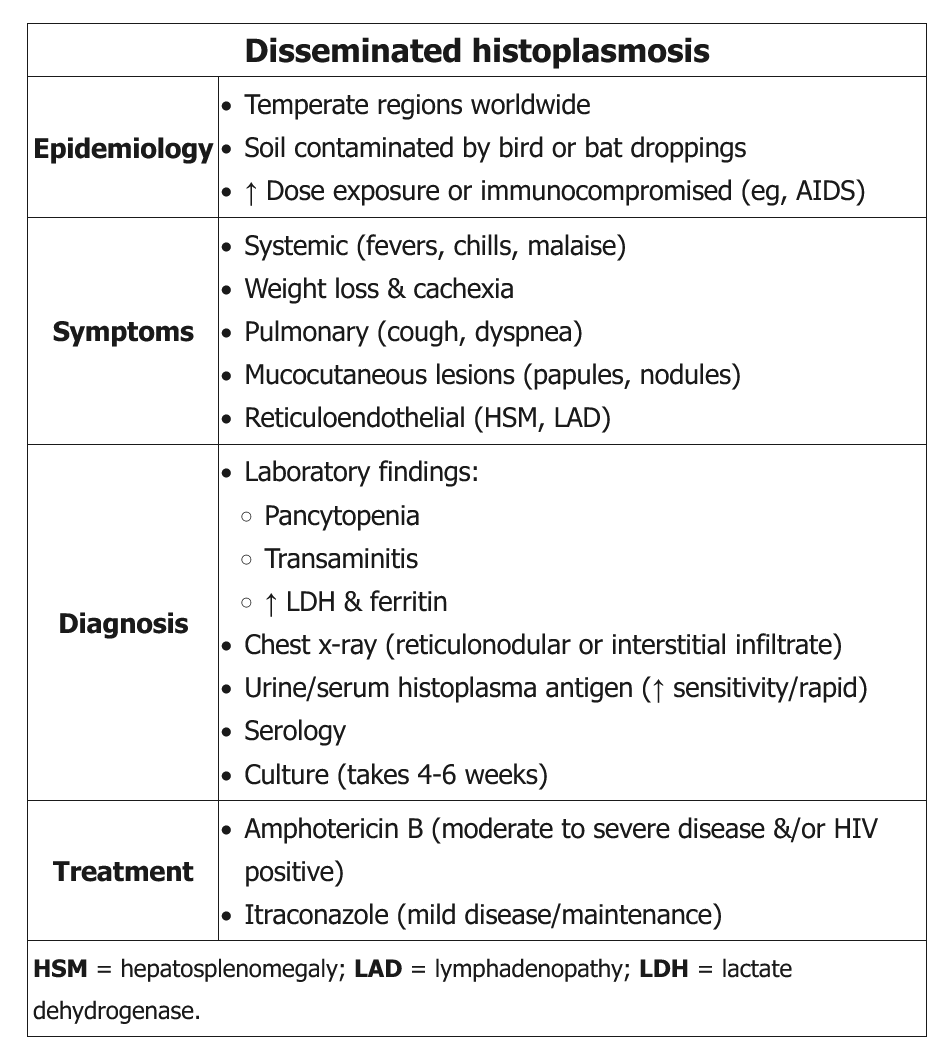
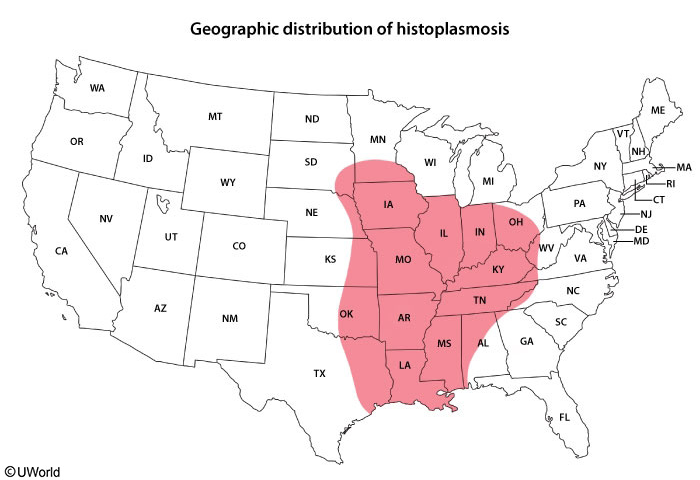
Histoplasma capsulatum is responsible for one of the most common endemic mycoses in the world. Acquired by inhalation of airborne conidia, this organism primarily produces asymptomatic pulmonary infection. It is distributed along the Mississippi River Valley (Ohio, Missouri, Indiana, Mississippi) in the United States, in Central and South America, in the Caribbean, and in regions of Africa, Australia, and India.
Histoplasmosis most commonly presents with acute respiratory symptoms. Other presentations, in declining order of frequency, include asymptomatic infection, disseminated infection, chronic pulmonary symptoms, rheumatologic symptoms, pericarditis, and sclerosing mediastinitis.
The Histoplasma urinary antigen assay has a sensitivity and specificity of greater than 85% in acute and disseminated infection but less than 50% in chronic infection. Identification of the fungus by tissue culture can be a lengthy process but is indicated for clinically suspected cases in which the urinary antigen assay result is negative.
Asymptomatic and mild pulmonary histoplasmosis typically resolves without treatment. Antifungal therapy is recommended for more severe or disseminated disease. Itraconazole is the agent of choice; duration of therapy is 6 to 12 weeks for acute infection and as long as 12 months for chronic cavitary pulmonary infection. For severe lung disease and disseminated infection, liposomal amphotericin B should be used initially, followed by de-escalation to oral itraconazole for an additional 12 weeks.
The most appropriate treatment for this patient is liposomal amphotericin B. He has disseminated histoplasmosis, for which he has numerous risk factors. He lives in an area endemic for histoplasmosis (Ohio River Valley), and because he takes prednisone and methotrexate for his rheumatoid arthritis, he is immunosuppressed. He has had significant exposure working in an old barn with bats. He also is hypotensive and diaphoretic and has oral ulcerations and hepatosplenomegaly, which are typical of disseminated infection, as is pancytopenia. Approximately 10% of patients with histoplasmosis develop disseminated infection; if not diagnosed early, the mortality rate is greater than 90%. The treatment of choice for disseminated histoplasmosis is liposomal amphotericin B initially, with de-escalation to itraconazole for several months. A definitive diagnosis can be established by detection of the urinary antigen for histoplasmosis (95% specificity), blood cultures, or a biopsy of the oral lesions.
Ceftriaxone and azithromycin are the recommended drugs of choice for community-acquired pneumonia. The patient's physical examination and chest radiograph are unremarkable, which effectively rules out pneumonia and the need for these antibiotics.
Behçet syndrome is a form of vasculitis associated with recurrent painful oral and genital ulcerations; patients also may demonstrate additional distinctive features, including hypopyon and pathergy. Central nervous system involvement can manifest as headaches, stroke, and behavioral changes. Gastrointestinal involvement may be hard to distinguish from inflammatory bowel disease. Low-dose prednisone or colchicine is used for oral or genital ulcers, and high-dose prednisone and immunomodulating agents are used for more severe disease. Behçet syndrome does not explain the patient's fever, hemodynamic instability, pancytopenia, or hepatomegaly, and colchicine therapy is not warranted.
Itraconazole is an azole triazole used to treat many endemic fungal infections, including histoplasmosis. However, it is not as effective as liposomal amphotericin B in disseminated infection. It may be used for subacute or chronic histoplasmosis, such as pulmonary histoplasmosis.