hepatopulmonary syndrome
- related: GI, Pulmonology
- tags: #pulmonology
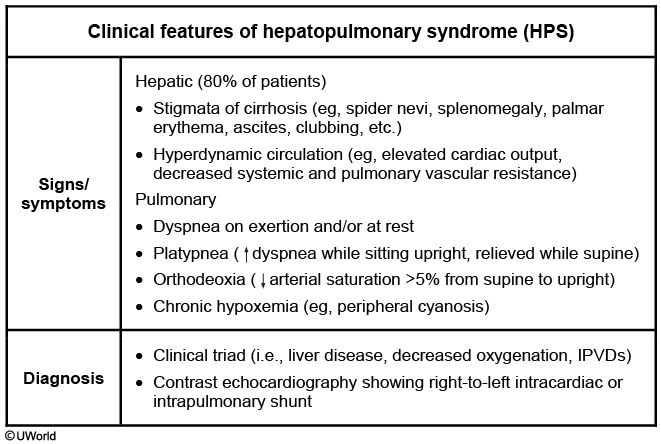
Hepatopulmonary syndrome is a complication of cirrhosis caused by dilation of the pulmonary vasculature in the setting of advanced liver disease and portal hypertension. A high alveolar-arterial oxygen gradient results from functional shunting. Patients with hepatopulmonary syndrome usually have a preexisting diagnosis of liver disease and present with shortness of breath. Dilation of pulmonary vasculature occurs at the base of the lungs, so hypoxemia is most noted when patients are upright or sitting, when shunting is maximal. Classic features are platypnea (worsening shortness of breath in the upright position) and orthodeoxia (worsening arterial oxygen saturation in the upright position). Pulse oximetry is often used to screen for changes in the arterial oxygen saturation level with changes of position. The diagnosis is made by demonstrating an arterial oxygen tension less than 80 mm Hg (10.7 kPa) breathing ambient air, or an alveolar-arterial gradient of 15 mm Hg (2 kPa) or greater, along with evidence of intrapulmonary shunting on echocardiography with agitated saline or macroaggregated albumin study. The detection of intrapulmonary shunting of blood is best confirmed by echocardiography with agitated saline (also known as a bubble study), during which bubbles are identified in the left side of the heart after 5 beats, demonstrating that the shunting of blood is not intracardiac. Clinically significant hepatopulmonary syndrome is treated with supplemental oxygen and liver transplantation. Hepatopulmonary syndrome is a progressive condition that is ultimately fatal without liver transplantation.
Hepatopulmonary syndrome is seen in 5%-40% of chronic liver disease patients. It is associated with portal hypertension, and usually presents years after the onset of chronic liver disease of any etiology. Patients typically present with the classic triad of liver disease, hypoxemia, and intrapulmonary vascular dilatations (IPVDs). IPVDs cause right-to-left shunting, which results in cyanosis and hypoxemia.
The IPVDs can be demonstrated by contrast enhanced echocardiography (best method), nuclear scanning (more expensive, less sensitive), or pulmonary angiography (invasive, seldom preferred). Contrast echocardiography (eg, with agitated saline; "bubble study") confirms intrapulmonary right-to-left shunt if the microbubbles passing through the dilated pulmonary vessels cause left heart opacification 3-6 heart beats after right heart opacification. There is no effective medical therapy for HPS, and liver transplant is recommended for patients with severe hypoxemia.