heparin induced thrombocytopenia and thrombosis
- related: Hemeonc
- tags: #hemeonc
type 1 HITT
- within 2 days of initiating heparin
- transient, non pathologic
- Plt > 100k
- Do not stop heparin, plt will return to normal
type 2 HITT
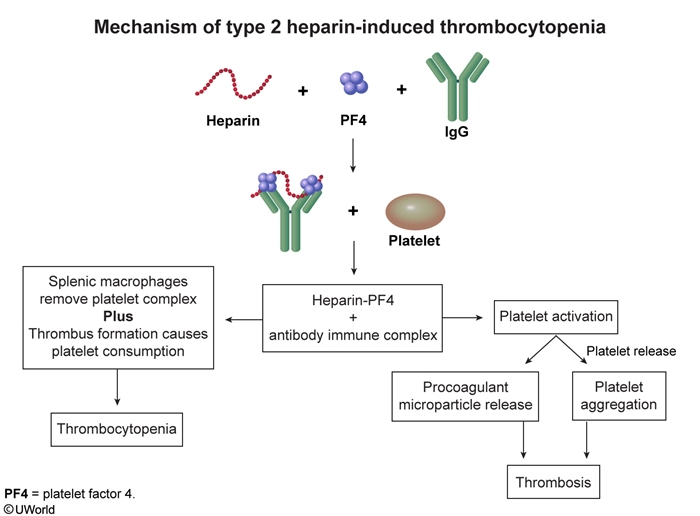
- antibody against PF4 => activates Plt => plt cascades => thrombosis and thrombocytopenia
- risks
- women
- most often unfractionated heparin
- CV surgery, ortho surgery, increased trauma severity
- more or longer heparin => more likely to get HITT
- patients with endothelial damage
- clotting is worse than bleeding
- arterial and venous clot
- Thrombocytopenia - platelets typically decline >30%-50%
- Timing - onset 5-10 days after heparin initiation or <1 day with prior, recent heparin exposure
- Thrombosis - new thrombosis, progressive thrombosis, or skin necrosis
- Alternative causes - no other sources for thrombocytopenia are present or likely
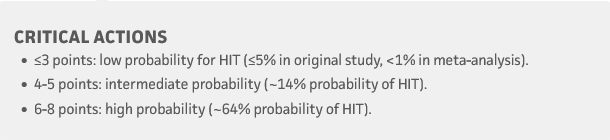
- interpret based on 4T score
- e.g. low 4T with positive test: 1% chance positive HITT
- Diagnosis is confirmed with serotonin release assays (preferred), heparin-induced platelet aggregation assays, or solid-phase immunoassays with ELISA for heparin-PF4 complexes.
- Stop argatroban: when Plt > 150k, then switch to DOAC or warfarin for minimum of 6 months. Initial treatment with warfarin is contraindicated as rapidly dropping protein C levels cause a prothrombotic state. Warfarin is usually started after the patient is treated with a non-heparin anticoagulant and recovers a platelet count to > 150,000/µL.
Delayed onset HIT
Delayed-onset HIT - immune mediated due to high-titer antibodies against heparin-PF4 complexes in the absence of circulating heparin. Cases typically arise 5-19 days after heparin cessation; therefore, most patients present in the outpatient setting. Thrombocytopenia with or without life-threatening arterial or venous thrombosis are the norm.
[!NOTE] extensive DVT with thrombocytopenia after major surgery in clinic