headache
- related: Neurology
- tags: #note
Approach to the Patient with Headache
- 3 headache types
- primary headaches: specific disorder
- migraine, tension, cluster, trigeminal neuralgia
- secondary headaches: underlying process. Acute or subacute. Progressive or unstable
- posttraumatic, whiplash
- ischemic, TIA, cervical artery dissection, sinus thrombosis
- bleeding: SAH, SDH
- spontaneous intracranial hypotension
- hypo/hypertension, sarcoid, neoplasia
- substance withdrawal
- infection
- MSK
- acute closed angle glaucoma
- hydrocephalus
- pheochromocytoma
- psychiatric
- painful cranial neuralgias
- primary headaches: specific disorder
secondary headache red flags:
- First or worst headache
- Abrupt-onset or thunderclap attack
- Progression or fundamental change in headache pattern
- Neurologic deficit
- New headache in persons older than 50 years
- New headache in patients with malignancy, coagulopathy, immunosuppression, or pregnancy
- Headache triggered by position, exertion, sexual activity, or Valsalva maneuver
Imaging
- MRI W
- uncommon primary headaches like trigeminal autonomic cephalalgias
- chronic headache with new or progressive features
- MRI WWO/CT WO: headache with optic disc edema or with clinical red flags
- CT WO: for thunderclap headaches
Thunderclap Headache
- severe headache pain
- abrupt onset
- maximum intensity in 1 min
- CT head WO 1st line dx
- LP: for opening pressure, cell count, xanthochromia if head CT nondiagnostic
- CTA or MRA: next if normal CT and normal CSF
- Ddx
- Subarachnoid hemorrhage: most common
Subarachnoid hemorrhage
- subarachnoid hemorrhage, SAH
- sx
- worst headache ever experienced (low specificity)
- increased risk:
- 40 years or oder
- onset during exertion
- witnessed LOC
- concominant neck pain
- sentinel leak (warning leaks)
- past headaches
- abrupt, severe, transient
- global or focal
- dx
- CT head: 95% sen at 12 hours but decreases to 50% at 1 week
- LP
- CSF RBC > 10,000 per microL
- elevated CSF protein
- xanthochromia: takes 4 hours to develop but nearly 100% sensitive between 12h-7days
Intracranial vein and sinus thrombosis
- 2 types
- cavernous sinus thrombosis: from bacterial infection, usually related to dental procedures
- other forms: usually thrombosis from hypercoatulation and not infection
- sx
- from increased intracranial pressure
- headache
- sudden onset, unremitting
- worse with valsava
- pulsatile tinnitus
- diplopia
- nonspecific findings: papilledema, decreased mentation, seizure, CN6 palsy from pressure
- cavernous sinus thrombosis:
- acute onset headache, proptosis, periorbital edema, ophthalmoplegia
- immediate abx with surgical drainage
- other forms of cerebral venous thrombosis
- anticoagulation, even in patients with hemorrhagic parenchymal lesions
- LMWH > unfractionated heparin
- Then warfarin for 3-6 months minimum
Cervical Vessel Dissection
-
pt: usually younger pt, could be trauma related
-
risks:
- HTN, migraine, PCOS, connective tissue disorder
-
sx
- head and neck pain
- carotid artery: orbital pain
- partial Horner syndrome: ptosis/miosis
- ipsilateral signs of cerebral/retinal ischemia
- vertebral artery:
- occipital and neck pain
- posterior fossa sx: dysarthria, dysphagia, ataxia, hemified visual loss
- MRI: tapered arterial lumen, increased arterial diameter with intramural hematoma
-
dx
- MRA/CTA
-
rx: many area treated with ASA. AC may not be superior
-
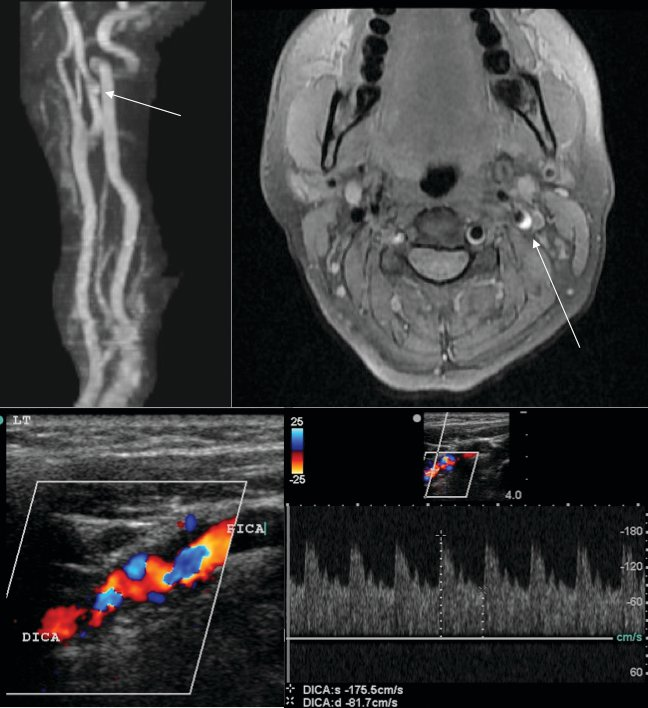
L ICA dissection, 32 year old woman, left frontal cerebral infarct
-
top left: MRA, mild irregularity, maybe aneurysm
-
top right: T1 MRI soft tissue, hematoma
-
bottom: carotid duplex, turbulent flow with increased velocities
Reversible cerebral vasoconstriction syndrome
- multifocal constriction of intracranial vessels normalizing in 3 months of onset
- second most common reason for thunderclab headache
- sx
- recurrent thunderclap headache
- triggered by exertion, valsalva, emotion, bathing
- minority of people: focal deficits, encephalopathy, seizures
- dx
- MRA/CTA of brain/neck vessels
- CSF analysis
- LP: typically normal
- brain MRI more sensitive and may show white matter edema areas in occipital and parietal lobe
Reversible cerebral vasoconstriction syndrome is characterized by recurrent thunderclap headache and multifocal constriction of intracranial vessels normalizing within 3 months of onset. Predisposing factors are listed in Table 4. It is the second most frequent source of thunderclap headache. The headaches may be triggered by exertion, Valsalva maneuvers, emotion, or bathing. Focal deficits, encephalopathy, and seizures are seen in a minority of patients. Diagnostic evaluation should include noninvasive imaging of the brain and neck vessels with MRA or CTA and CSF analysis. Digital subtraction angiography has been associated with transient neurologic deficits and is typically avoided. Results of head CT and lumbar puncture are both typically normal. Brain MRI is more sensitive and may show areas of white matter edema primarily in the occipital and parietal lobes compatible with posterior reversible encephalopathy syndrome. Areas of ischemia or hemorrhage may be seen in the parenchyma, and a subdural or subarachnoid hemorrhage also may be found in some patients. Management begins with resolution of predisposing factors, avoidance of physical exertion, and management of blood pressure. Verapamil and nimodipine are the drugs of choice. Glucocorticoids may worsen the clinical course and should be avoided. Repeat MRA or CTA is necessary at 12 weeks to document resolution of vasospasm, at which time medication is tapered.
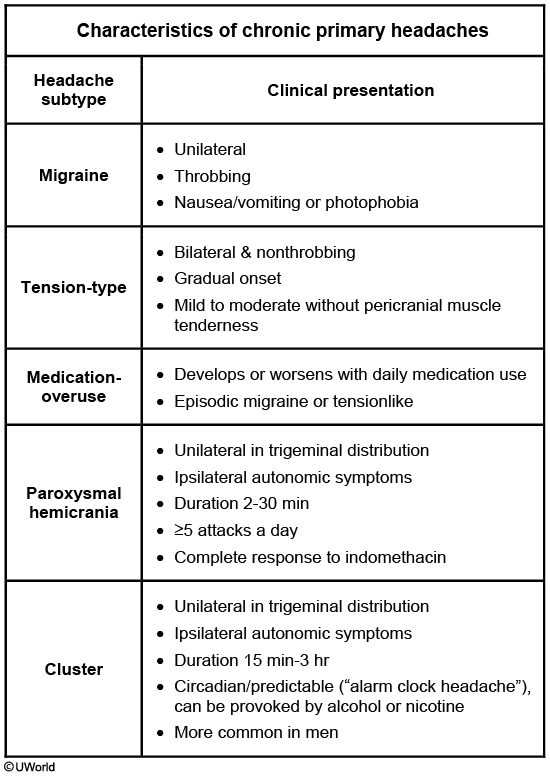
Paroxysmal hemicrania
This patient likely has paroxysmal hemicrania, an episodic or chronic headache disorder. Patients typically have frequent episodes of unilateral throbbing head pain (>5 attacks a day) that usually last 2-30 minutes and are associated with autonomic features (ipsilateral lacrimation, conjunctival injection, and miosis). Improvement with indomethacin is a diagnostic criterion. An MRI of the brain is needed to rule out intracranial pathology. Paroxysmal hemicrania can turn into a chronic headache disorder known as chronic paroxysmal hemicrania (daily headache with pain-free periods) or hemicrania continua (daily headache without pain-free periods).
Paroxysmal hemicrania, hemicrania continua, and cluster headache are considered trigeminal autonomic cephalalgias (characterized by unilateral trigeminal pain with associated ipsilateral autonomic findings). The main features of paroxysmal hemicranias that differentiate them from cluster headaches are higher frequency and shorter duration of attacks and response to treatment with indomethacin. Cluster headaches are more common in men, tend to follow a circadian rhythm, and can be triggered by small amounts of alcohol or nicotine. Migrainous features (eg, photophobia, phonophobia, nausea) are usually absent in paroxysmal hemicrania; furthermore, migraine headaches almost always switch sides, often migrate, and typically last 4-72 hours (Choice C).