goals of care
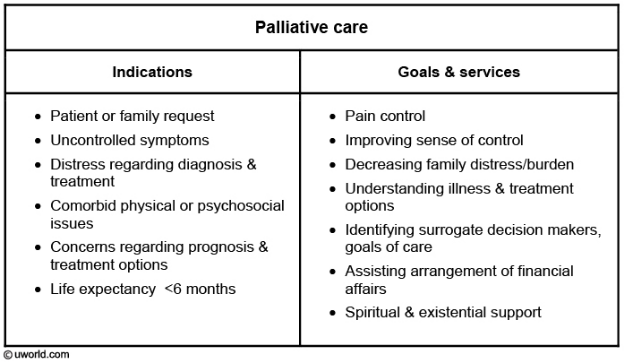
- related: Medicine, palliative care, MOST form
- tags: #note
Quick Overview
- Introduction
- Always introduce yourself and the team before big family discussions
- Make sure burning questions to be answered
- Keep at top level, don't jump to answer specific questions in the beginning
- Assess emotion at each level. Don't proceed if you sense resistance or unnamed emotions
- Start with emotion, build rapport
- We can't imagine how hard it is for you
- How are you coping?
- breakdown => explore emotions, stop
- doing ok => keep going
- Assess disease understanding
- What is your understanding
- Tell me what you've been told
- Assess prognostic awareness
- Assess for values
- Has he/she ever indicated to you what would be unacceptable level of suffering?
- For example, some people... no nursing home
- Others would say, keep going no matter what
- What about artificial nutrition
- Pause for transition
- Is it ok if we talk about prognosis
- Would it be ok if I share my biggest worry
- Hope/worry statements
- Assess for value specific to prognosis once they have good understanding. Do not proceed if they have poor understanding of disease and prognosis
- Some people would say considering everything they've been through, they would opt to go for comfort and not suffering
- Others would keep treating with everything in reasonable fashion to prolong life
Words to use
- To get answer for the near future:
- We are worried your ___ is getting sicker. There may come a time when he/she need to be moved to the ICU and even may require mechanical support.
- Patient may die soon:
- I'm worried despite our best efforts, your loved one may die in the near future. What would be helpful for us to know is that if that were to happen, what your loved one would say
- Some people want heroic measures to bring them back to life
- Some people would want to be comfortable in that case and allow them to pass away peacefully
- I'm worried despite our best efforts, your loved one may die in the near future. What would be helpful for us to know is that if that were to happen, what your loved one would say
- I recognize this is a tough place to be. I don't expect any decisions to be made today
Overview
- Know the headliner: one liner that summarizes his status short term or long term
- Start with value
- ask about what they were like before
- "Would it be ok if I tell you what I'm worried about?"
- "Our hope is…" (to get him back to doing what he was doing before)
- "I'm worried about…" (what's the main problem here in the hospital)
- Best case scenario… ("he may never do those things again and spend the rest of his life in a nursing home")
- Worst case scenario…
- then leave it here. Pause to assess response
- ask "what do you think about that?"
- agreement => "it sounds like he is being kept a live for the sake of being alive and not being able to do…" "I'm worried our options are…"
- "God will pull him through" => "tell me more," "what does that look like?", "what we hope to see is, but we are worried that…"
- Silence/overwhelmed => empathy statements, "no decisions need to be made today," "what other people have done in this situation," "primary team may do this and ask you this," hope/worry statements, "time may be more limited than we could hope," "we may need to make more decisions in the next few days"
Code Status
- have you done any advanced care planning prior to come to the hospital
- that's great you've made decisions like that. What helped you make those decisions
- Have you been through similar situations with a loved one that dealt with illnesses. Did you have to make those decisions
- Have you been asked about CPR before
- If something happened, and you died. Your heart stopped, and you stop breathing. I'd like to talk to you about the outcomes about CPR. If that's ok
- In general 25% leave the hospital. In your case, only 7 people in about 100 live
- Here's what we are going to do: abx, struggle to breath = intubation. But if you were to die, we will leave you at peace.
ATA
- Ask
- Tell
- Ask
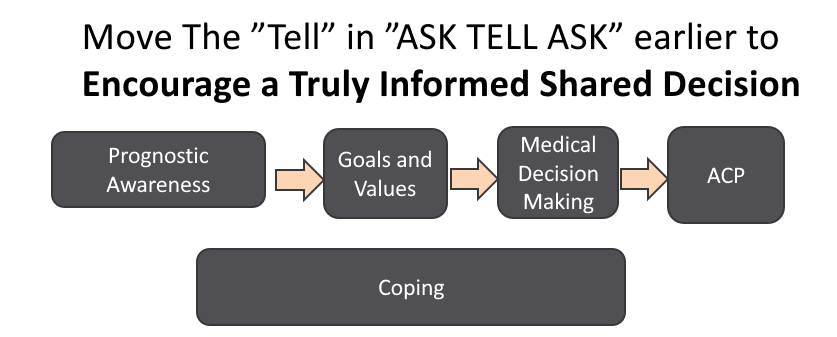
- prognosis drives perspective
Spikes
- setting
- introduce a purpose, prepare for decisions
- ask permission
- I’d like to talk about what is ahead with your illness and think about what is important to you so we can provide the best care possible that you want. I would like to do this with someone you consider to be your decision maker. Is this ok?
- perception
- their understanding of current illness
- are they comfortable making big decision about the direction of care, with my professional opinion as guide
- "many people have difficulty making big decisions for loved ones. It can be very stressful. How are you doing"
- assess prognosis and certainty of prognosis
- assess family preference for role in decision making
- invitation
- Invitation to go over difficult information
- knowledge
- Share prognosis
- Warning shot: What I am about to say may be hard to hear…
- explain what is happening medically in simple terms
- keep short, 3 main points
- Frame as a “wish…worry”, “hope...worry” statement
- Uncertain: "It can be difficult to predict what will happen with your illness. I hope you will continue to live well for a long time and I’m worried that you could get sick quickly, and I think it is important to prepare for that possibility."
- "I wish we were not in this situation, and I am worried that time may be as short as ___ (express as a range, e.g. days to weeks, weeks to months, months to a year)."
- Function: "I hope that this is not the case, and I'm worried that this may be as strong as you will feel, and things are likely to get more difficult."
- emotion
- Allow silence, explore emotion
- Pause and say this is the hardest thing you have to say to them today.
- I want us to think about how this information affects what is important to you
- Explore goals and values
- What are your hopes and worries about your health
- Assesses prognostic awareness
- Most people want a life that allows certain goals to be accomplished, such as communicating with loved ones, and not being completely dependent on others and living in a nursing home. How do you feel about these things? Do you have other examples of important goals for you?
- What abilities are so critical that you can’t live without them?
- What gives you strength as you deal with this?
- What matters to you most in this time in your life?
- Have you already made significant decisions or did important paperwork before? What did it say and Why?
- Have you known someone else who was very sick and did it lead to decisions about what you want for yourself?
- Do you want us to do aggressive things with very little chance of benefit and a high chance of harm?
- Do you want us to do things to live longer even if it could mean being on machines long term w/o the ability to interact with loved ones?
- summary
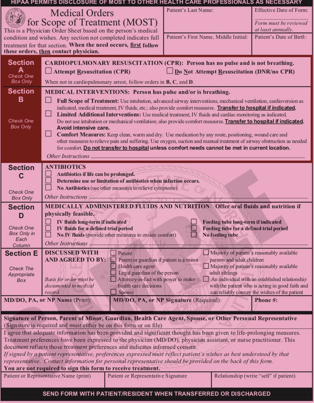
Advanced Care Planning
- Would you be surprised if this patient died in the next year?
- Use e-prognosis for prognostic range
- If not surprised:
- suggest goals of care with decision maker present if possible
- assess understanding, fill in knowledge gap
- give a prognosis with warning shot
- explore goals
- informed consent life prolonging measures
- put this all together with their values
- identify a decision maker
- document who the person is
Keys to ICU
- Bridge expectation between what family think will happen and what we think will happen
- What would be the quality of life if patient were to survive
- physical and cognitive debility
- what would the patient want if he knew what was happening
- More MD listening than talking
- Non-abandonment statements
- assurance of care for suffering
- supportive, empathetic statements
He would want everything done
- What concerns are driving this statement?
- Protecting their loved one
- Mistrust?
- Will other family perceive that enough is being done?
- Will we be less vigilant if changed to a DNR?
- One study found DNR led to less DVT prophylaxis
- Do they know the true prognosis?
- Your response: "Of course you do. He deserves the best care possible. We can only do that by informing you about what is likely to come, even with the best care possible. Can we talk more about that?"
- "Everything" Usually means one of the following:
- Everything that has a reasonable change of prolonging life, but not if it would increase suffering
- Or…even if it may cause a modest increase in suffering
- Or…lengthen life regardless of effect on suffering
- Or…even if decreasing suffering may unintentionally shorten life
Comfort Care Discussion
- There is nothing wrong with stopping life support
- Non-Abandonment Statements
- They will need direction and guidance
- Give a professional opinion in light of values/goals
- Normalize that it is ok to stop life support
- Stopping treatment is allowing nature to take its course, for a natural death to occur. We are not playing God
- Catholic doctrine shaped hospital ethics:
- Only wrong to stop life support if it will work really well to provide a long life, AND it is not leading to suffering
- Keep it to two or three options if possible:
- Aggressive care vs focusing on comfort, two paths
- Not “withdrawing care”
- Assurance of care for suffering
- Have to explain what comfort measures looks like:
- Pain medication used to trick the brain into thinking “I don’t feel short of breath”
- Only used to decrease shortness of breath, not to stop breathing or shorten life
- Being off machines, sleeping comfortably while you spend time with him
- But a focus on comfort can mean less time alive, and that’s ok
Time Limited trial
Trying something for a defined period of time with a preferred outcome:
- What is the goal?
- 5 days on the ventilator after cardiac arrest waiting for improved cognition
- 5 days on the ventilator to look for improved vent settings
- If this does not occur, plan on focusing on comfort
Empathy Statements
- Beginning:
- how are you doing
- are you getting rest
- Name emotions
- I realize this is a shock
- respect
- thank you for advocating for your loved one and having these difficult conversations with me
- supporting
- we will be here for you and guide you through this. You aren't expected to know what to do with these complex situations
- explore
- what do you need help with decisions about your loved one
More Expert Pearls
- This disease is leading to his death, not our decisions. Our decisions are about relieving suffering
- "Imagine your family member is sitting here, hearing about what his quality of life would look like. What would he tell us to do?"
- "This means you wrist band will change to No CPR. This does not change the care you receive now. It means if you die, we will let you be at peace."
- Affirm the decision
- "The decision you have made is a loving and logical decision for you and your family. I agree with your decision"