essential thrombocytosis
- related: Hemeonc
- questions to ask
- splenomegaly
- menstrual hx
- hx of clots
- family hx
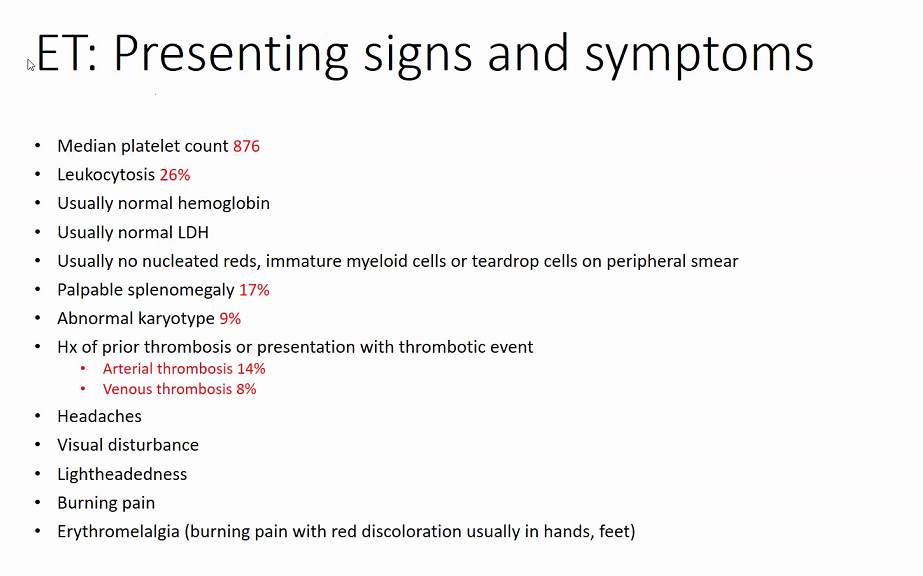
- sx
- labs
- iron profile
- esr/crp
- ldh
- uric acid
- JAK2: V617F, exon 12
- CALR
- MPL
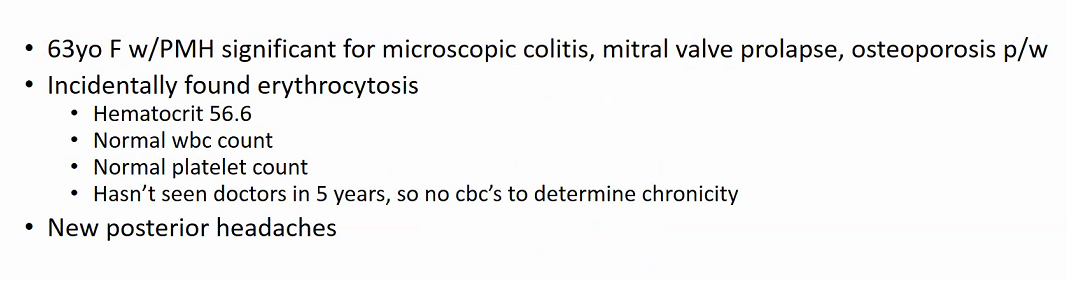
Patients with ET are often asymptomatic but can develop vasomotor symptoms (eg, headaches, dizziness, chest pain), thrombosis (eg, deep venous thrombosis), and/or hemorrhage (eg, mucosal bleeding). Physical examination often reveals splenomegaly. Hemoglobin and leukocyte count are typically normal. The diagnosis is confirmed with bone marrow aspirate/biopsy and testing for typical driver mutations; other myeloproliferative disorders (eg, chronic myeloid leukemia) must be excluded. Patients at low risk for thrombosis (age <60, no previous thrombosis) are treated with aspirin; higher-risk patients usually receive hydroxyurea.
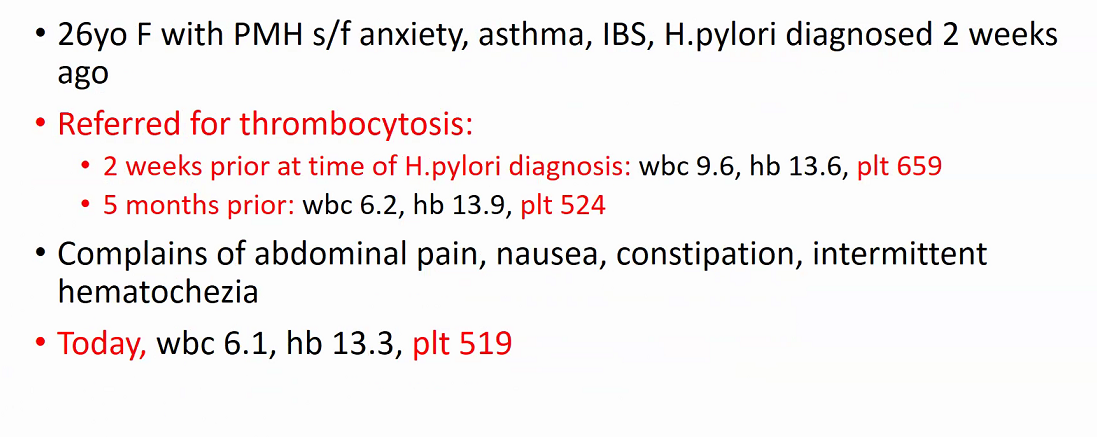
- ddx

- IDA
- infection
- inflammation
- post-splenectomy
Management
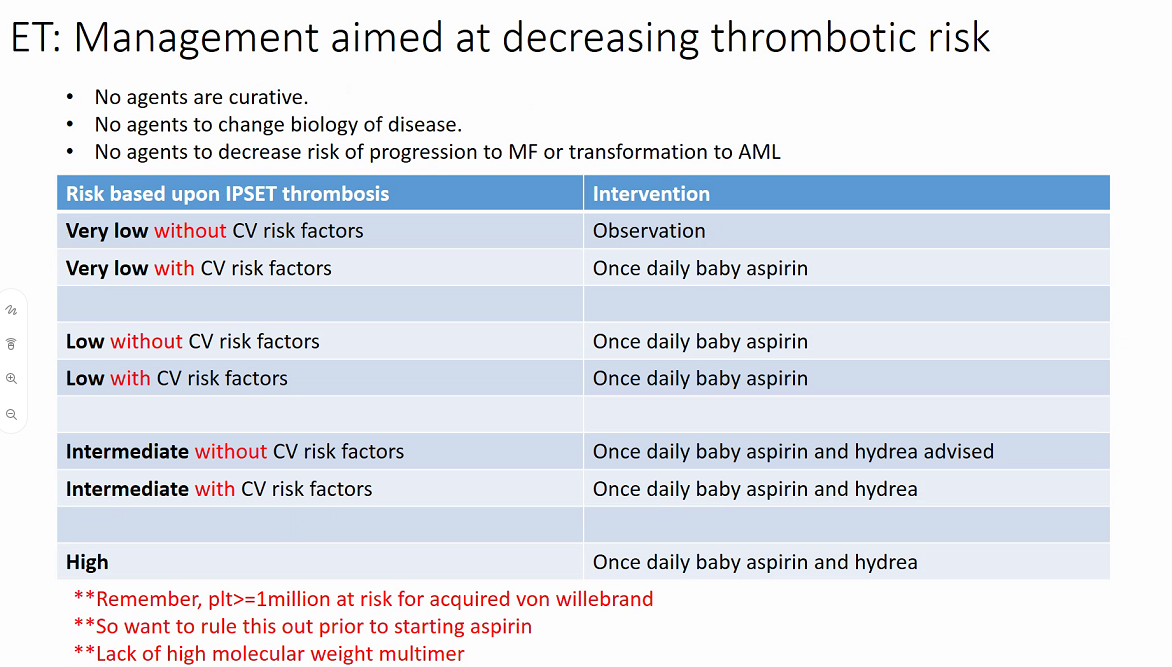
- rule out vWF with high molecular weight multimer
- hydrea is teratogenic and increases non-melanoma skin cancers
- alternatives
- anagrelide
- PEG-IFN
- busulfan
- ruxolitinib
Approximately 20% of patients with ET develop acquired von Willebrand disease (VWD). This is likely due to the consumption of large von Willebrand factor multimers secondary to platelet activation and proteolysis. Acquired VWD is associated with increased risk for skin and mucosal bleeding, which limit the ability to use aspirin for treatment. However, cytoreduction often resolves or improves the condition.
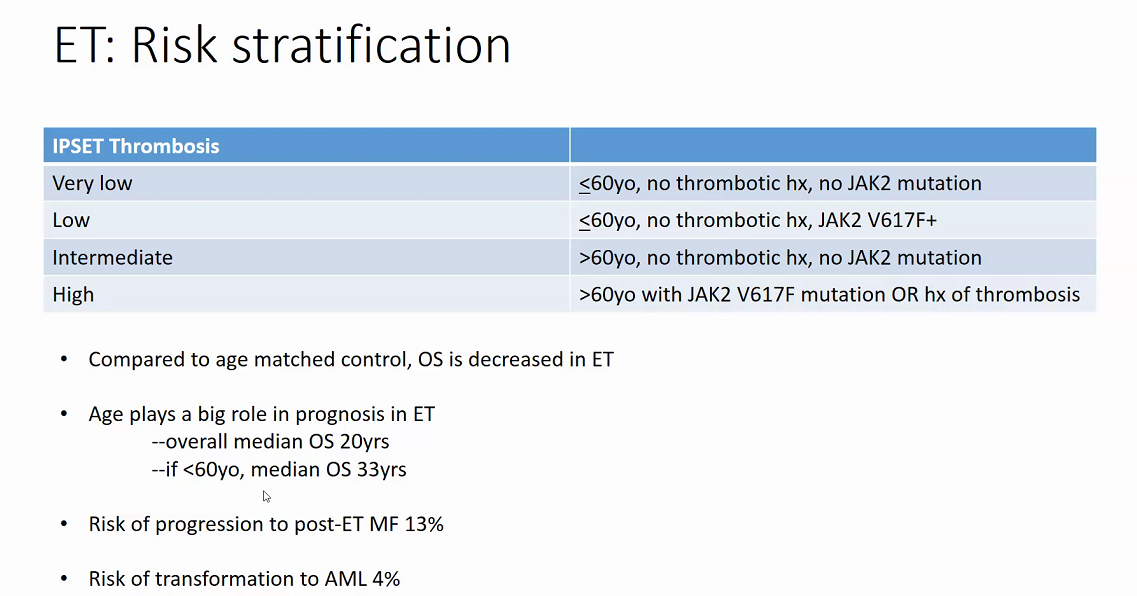
Prognosis