Ehrlichosis
- related: ID, tick born infections
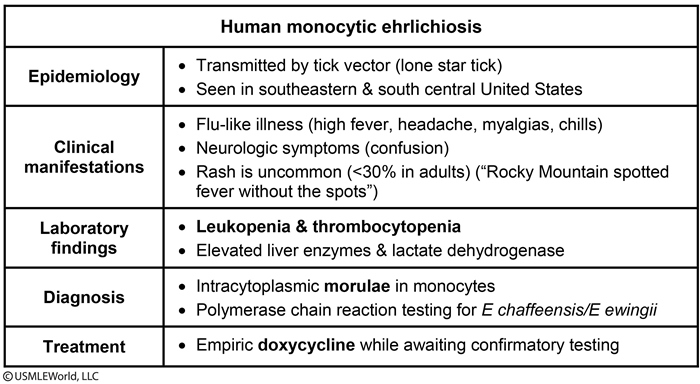
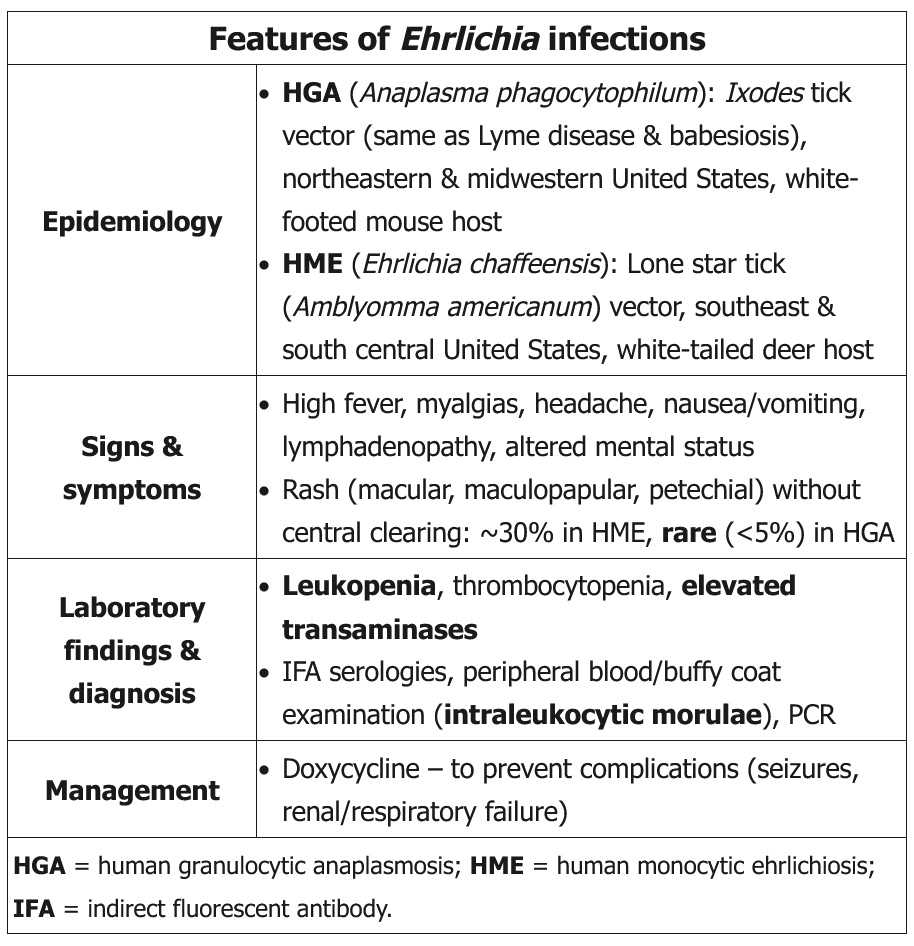
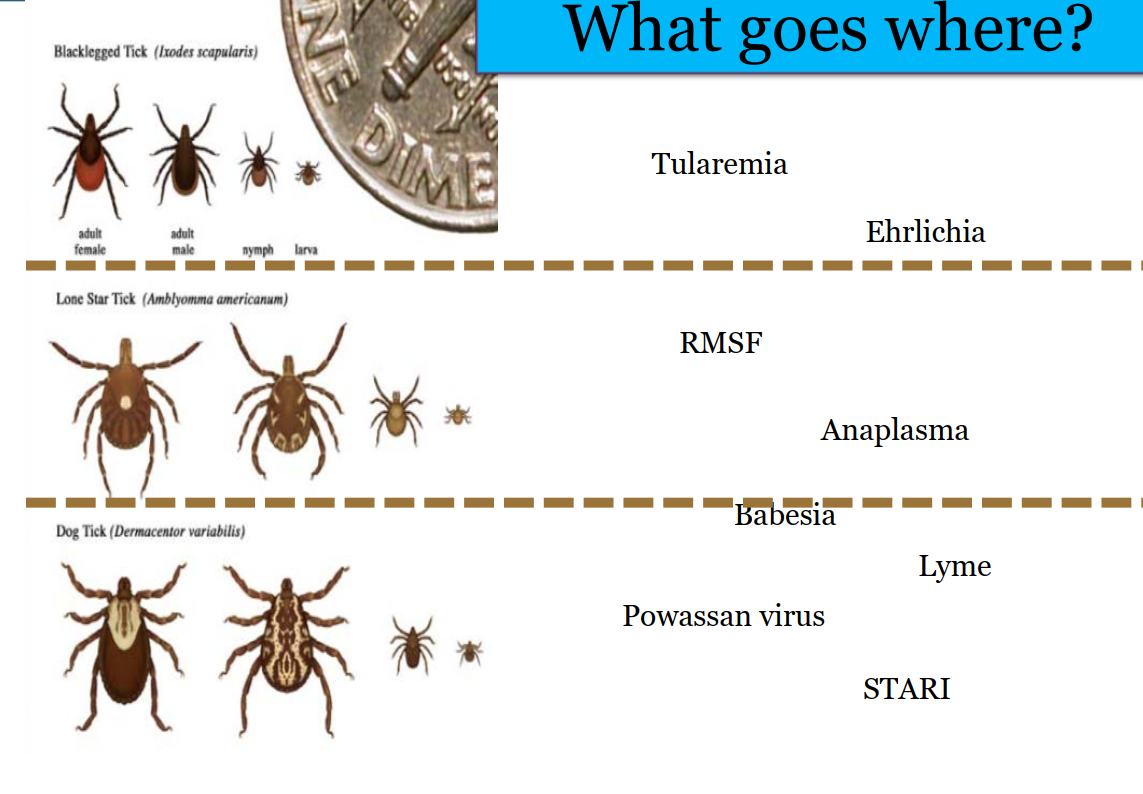
Ehrlichiosis is a tick-borne infection caused by Ehrlichia chaffeensis and E ewingii. These bacteria are carried by ticks, including the lone star tick (Amblyomma americanum), found in the southeastern and south central United States. The principal reservoir is the white tail deer.
HME typically occurs in the spring and summer months in the southeastern and south central United States. It is similar to human granulocytic anaplasmosis (HGA), another form of ehrlichiosis (seen primarily in the northeastern and midwestern United States and rarely associated with rash) that is transmitted by the Ixodes scapularis tick, which is also the vector for Lyme disease and babesiosis.
Ehrlichiosis is characterized by an acute febrile illness with malaise and altered mental status. Ehrlichiosis is not often associated with a rash (<30% in adults) and is described as "Rocky Mountain spotted fever (RMSF) without the spots." Neurologic symptoms may include confusion, mental status changes, clonus, and neck stiffness. Laboratory studies often show leukopenia and/or thrombocytopenia, along with elevated aminotransferases and lactate dehydrogenase.
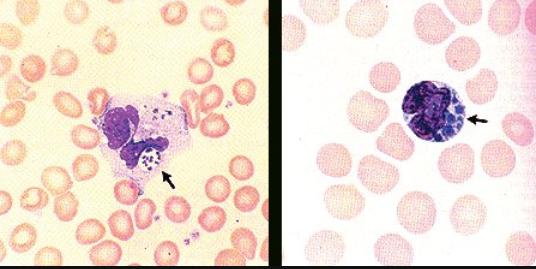
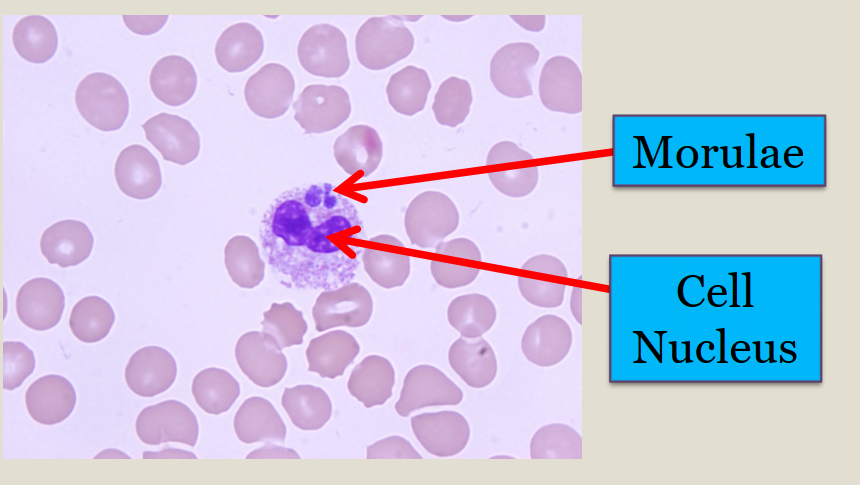
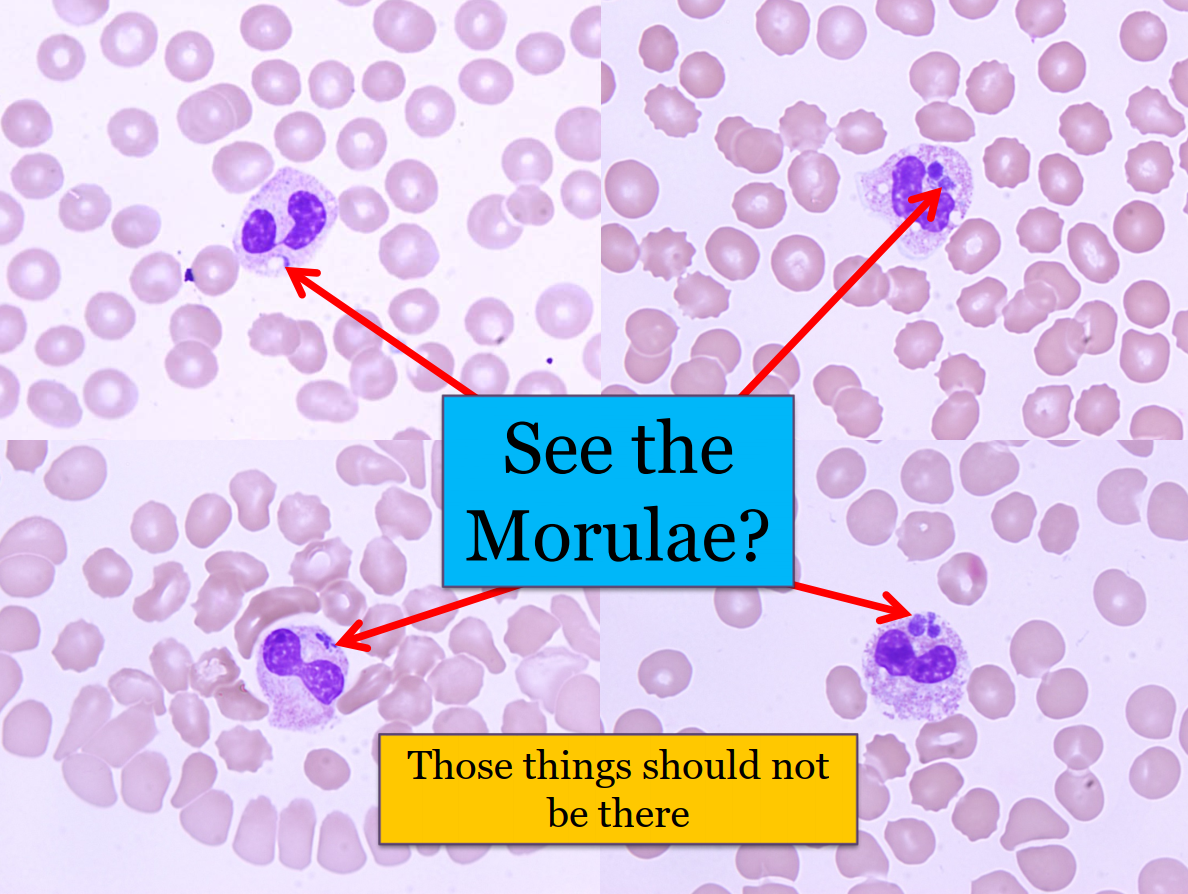
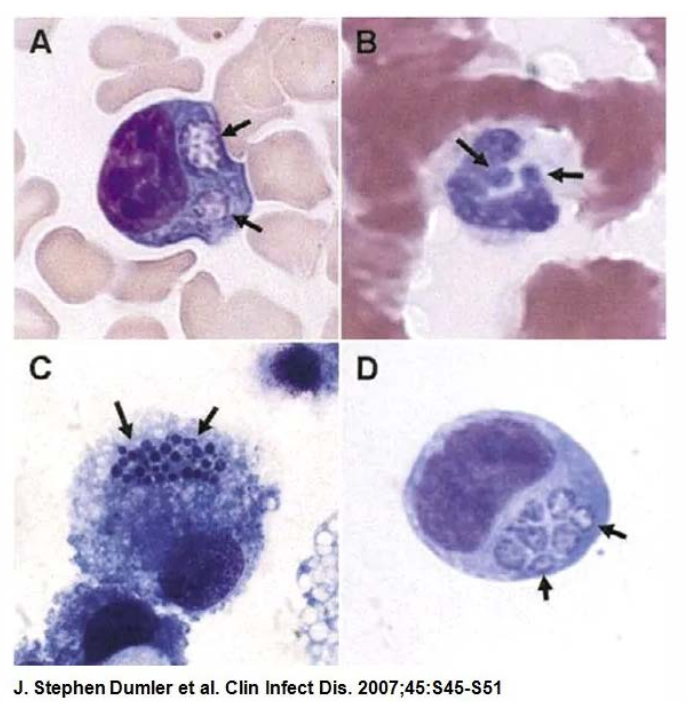
The diagnosis is often clinical, although definitive diagnosis can be made through visualization of intracytoplasmic morulae in white blood cells or through polymerase chain reaction testing. Doxycycline is the appropriate treatment and is often initiated empirically when the diagnosis is suspected while confirmatory testing is pending.
This patient most likely has human monocytic ehrlichiosis (HME), a tick-borne illness primarily caused by Ehrlichia chaffeensis. His symptoms include a nonfocal febrile illness associated with leukopenia, thrombocytopenia, and elevated hepatic enzyme levels, all of which are characteristic of HME. His participation in outdoor activities in wooded areas places him at risk for exposure to ticks. HME is endemic in the mid-Atlantic, southern, and southeastern United States; his clinical presentation is highly suggestive of this illness. The prompt response to doxycycline is classic for a tick-borne rickettsial illness, such as HME; a lack of response within 48 hours of therapy would suggest an alternative diagnosis or a coinfection. The negative serologic results for E. chaffeensis do not disprove the diagnosis and should not prompt early discontinuation of doxycycline. The sensitivity of antibody testing is low in the first week of illness; seroconversion typically occurs within 2 to 4 weeks of symptom onset, and acute and convalescent titers are useful for retrospective confirmation of infection. During the acute illness, buffy-coat staining (to reveal the presence of morulae, which are basophilic inclusion bodies in the cytoplasm of monocytes representing clusters of bacteria [shown]) or polymerase chain reaction of whole blood specimens may allow an early diagnosis.
Although many infections present identically to HME, the salient feature in this patient was the rapid response to doxycycline therapy, which essentially excludes a viral process. Heartland virus, a newly described Bunyavirus transmitted by the same vector as E. chaffeensis, is clinically indistinguishable from HME and should be suspected when no improvement is seen within 48 hours of starting doxycycline therapy.
Infectious mononucleosis can present with fever, cytopenia, and elevated aminotransferase levels. However, other components of the infectious mononucleosis triad (fever, pharyngitis, and cervical lymphadenopathy) were absent in this patient.
The rapid response to doxycycline treatment is consistent with Rocky Mountain spotted fever (RMSF) infection. However, the pronounced leukopenia and absence of a rash more than 1 week into the illness argue against this diagnosis.
Rickettsia rickettsii causes Rocky Mountain spotted fever (RMSF) and can look similar in its early stages to HME, but leukopenia is less common in RMSF. In addition, the RMSF rash (seen in 90% of patients) usually begins on the extremities.
- grow in intracellular vacuoles called morulae
Anaplasma
-
similar to Lyme location
-
same Ixodes tick
-
can have coinfection (erythema migran with fever, leukopenia, transminitis)
-
Midwest, NE
-
Ehrlichia: more in south
-
flu like
- fever
- myalgia
- headache
- cough slide: 62