dengue
- related: zika, dengue, chikungunya
- Dengue fever is the most prevalent arthropod-borne viral infection in the world. Endemic areas include Southeast Asia, the South Pacific, South and Central America, and the Caribbean.
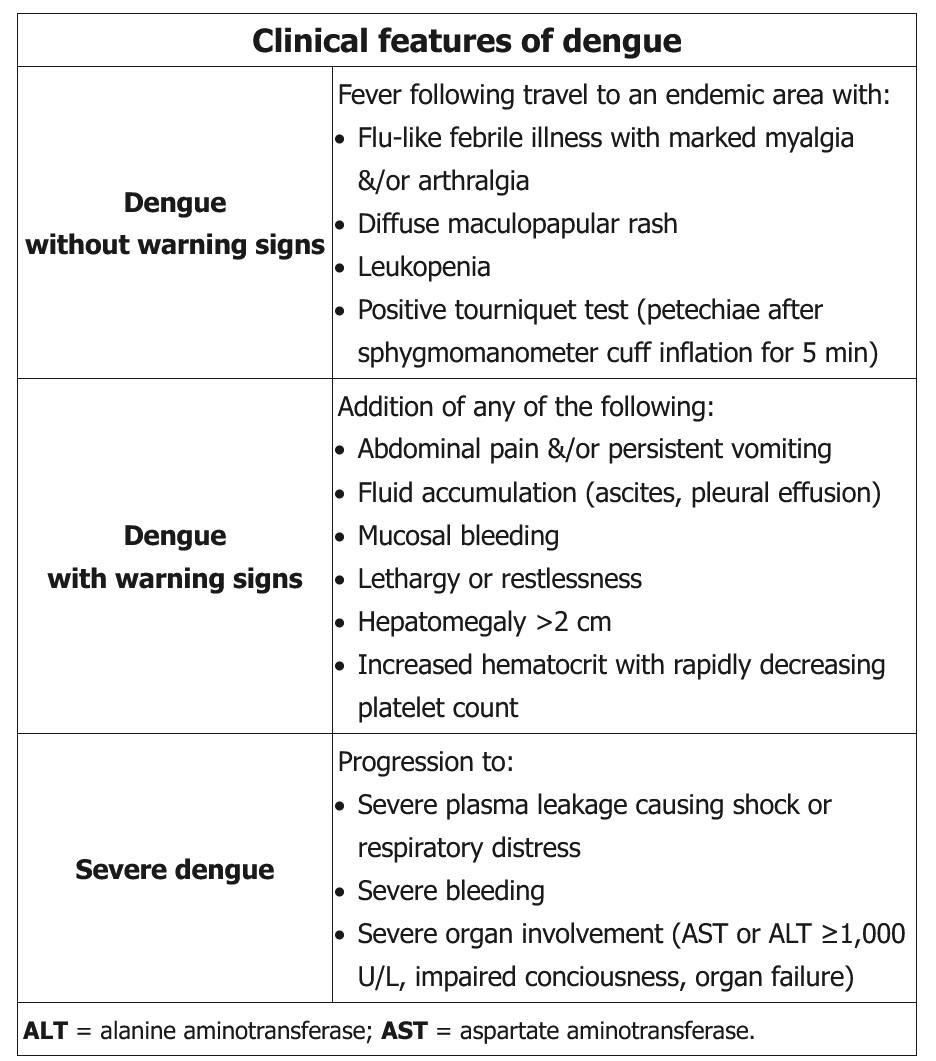
- The incubation period is 4 to 7 days. Patients may be asymptomatic or present with an acute febrile illness associated with frontal headache, retro-orbital pain, myalgia, and arthralgia, with or without minor spontaneous bleeding. Gastrointestinal or respiratory symptoms may predominate. Severe lumbosacral pain is characteristic. As the fever abates, a macular or scarlatiniform rash, which spares the palms and soles, may develop and evolve into areas of petechiae on extensor surfaces. Fever resolves after 5 to 7 days; however, some patients experience a second febrile period (saddleback pattern). A prolonged period of severe fatigue may follow. In patients with severe infection, life-threatening hemorrhage (dengue hemorrhagic fever) or shock may ensue, with liver failure, encephalopathy, and myocardial damage. This syndrome appears to be related to previous infection of a different serotype and is unlikely in travelers who have not had dengue fever previously.
- Abnormal laboratory findings include leukopenia, thrombocytopenia, and elevated serum aminotransferase levels. Diagnosis of dengue fever is based on clinical suspicion in a patient who traveled to an endemic area and presents with fever and other typical signs, symptoms, and abnormal laboratory findings. Diagnosis is confirmed by serology (IgM and IgG) or reverse transcriptase PCR.
- Therapy is supportive. A live attenuated dengue vaccine was approved by the FDA in May 2019. However, it is for use only in persons aged 9 to 16 years. Recipients must have laboratory-confirmed previous dengue infection and live in an endemic area.
Dengue fever (DF) is a common cause of fever in travelers returning from the Caribbean, parts of Asia, and South America. In addition to fever, the first period of illness (usually 3-5 days) is marked by myalgias, retro-orbital pain/headache, and bleeding complications (eg, epistaxis). As these symptoms improve, a characteristic macular or maculopapular rash ("islands of white in a sea of red") may appear. At around the same time, patients enter the critical phase of the illness; some may develop capillary leakage with edema, effusions, hypotension/shock, and severe hemorrhage. A positive tourniquet test may be seen (petechiae following sphygmomanometer inflation for 5 minutes over the arm). Laboratory abnormalities include leukopenia, thrombocytopenia, and an elevated hematocrit due to hemoconcentration (even in the absence of hemorrhage). Diagnosis is made via serology or direct testing for viral components, and care is largely supportive.