cystic fibrosis
- related: Pulmonology
- tags: #pulmonology
Diagnosis
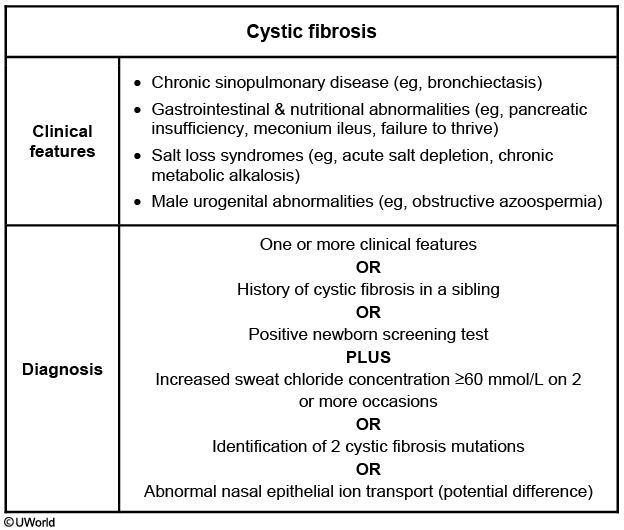
This patient's clinical presentation is suggestive of cystic fibrosis (CF). Cystic fibrosis is generally diagnosed in infants and children, but approximately 7% of patients are diagnosed after 18 years of age. Adult CF patients usually present with chronic respiratory problems often labeled as asthma, COPD, and recurrent bronchitis. Adults have milder lung disease with fewer pseudomonal infections than children and usually present with upper lobe bronchiectasis, recurrent pancreatitis, chronic sinusitis, or infertility (usually due to congenital absence of the vas deferens). Adult CF patients also tend to have nontuberculous mycobacterial infections, pancreatic insufficiency, and unusual genetic mutations.
Diagnosis is confirmed by sweat chloride test > 60 mmol/L on > 2 occasions, but adults may have equivocal results. Patients suspected of having CF with a normal or borderline sweat chloride test should then have a CFTR mutation analysis. Continued CF suspicion in patients without two CFTR mutations may require further workup with expanded DNA analysis or nasal potential difference measurement. This patient has upper lobe bronchiectasis with evidence of pancreatic insufficiency and should have a sweat chloride test for CF evaluation.
Allergic bronchopulmonary aspergillosis (ABPA) usually presents with moderate to severe persistent asthma, central bronchiectasis, elevated serum IgE, eosinophilia, and positive sputum cultures for Aspergillus species. Although up to 10% of CF patients can develop ABPA, this patient should first have a sweat chloride test to diagnose CF before further testing.
Common variable immunodeficiency can present in adults with repeated sinopulmonary infections or bronchiectasis. Fungal and tuberculous infections can also cause bronchiectasis. However, given the patient’s pancreatic insufficiency, he should first be evaluated for cystic fibrosis.