contraindications to air travel
- related: General
- tags: #note
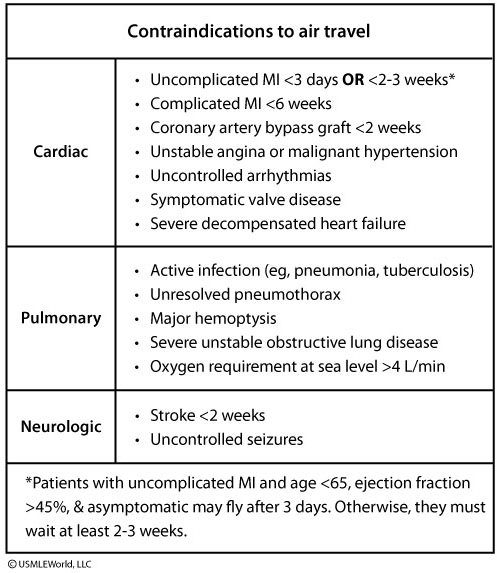
Decreased partial pressure of oxygen in pressurized cabins during airplane flights may increase the risk of hypoxemia in patients with pulmonary disease. Cabin altitudes are pressurized to 8000 feet, at which the fraction of inspired oxygen falls to 0.15 versus the normal 0.21 at sea level. This correlates to a drop in oxygen saturation to 89%-94% in healthy passengers. Most healthy individuals can compensate for this small degree of hypoxia. However, patients with severe unstable obstructive lung disease may not be able to compensate and can develop symptoms (eg, lightheadedness, chest pain, tingling in the extremities, palpitations, increased dyspnea).
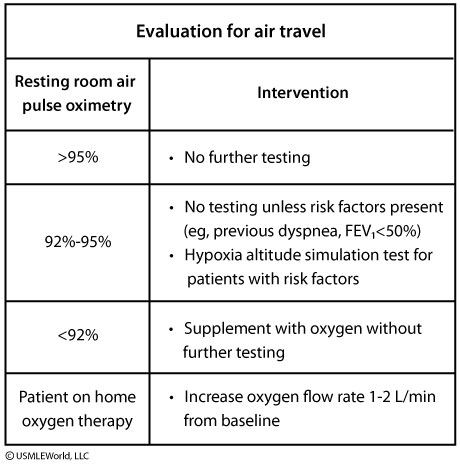
Forced expiratory volume in 1 second (FEV1) and pulse oximetry (SpO2) can help assess clinical severity of lung disease. Patients with SpO2 >95% are generally not at risk for in-flight hypoxemia and do not require further testing. Those with SpO2 of 92%-95% are also not at risk unless they have other factors (eg, previous dyspnea during air travel, inability to walk 50 m without respiratory distress, FEV1 <50%, or moderate to severe pulmonary hypertension). These patients require further testing and may need oxygen supplementation prior to air travel. Supplemental oxygen (2 L/min) is recommended during flights for patients with resting SpO2 <92%. If the patient is already on home oxygen, an increase of 1-2 L/min from baseline is recommended. This patient has stable chronic obstructive pulmonary disease with SpO2 >95% at rest and requires no supplemental oxygen or further testing prior to air travel (Choices A, D, and E).
A hypoxia altitude simulation test is used to predict in-flight hypoxemia when results of pulse oximetry are inconclusive. The test involves having the patient breathe in a mixture of nitrogen and oxygen at 15% (normal room air is 21%) for 20 minutes. In-flight supplemental oxygen is usually required if SpO2 levels are <85% (PaO2 <50 mm Hg) at any point during the test.