conjunctivitis
- related:eye problems
Conjunctivitis is a diagnosis of exclusion, and is made in a patient with red eye and discharge only if vision is normal and there is no evidence of glaucoma, iritis, or keratitis.
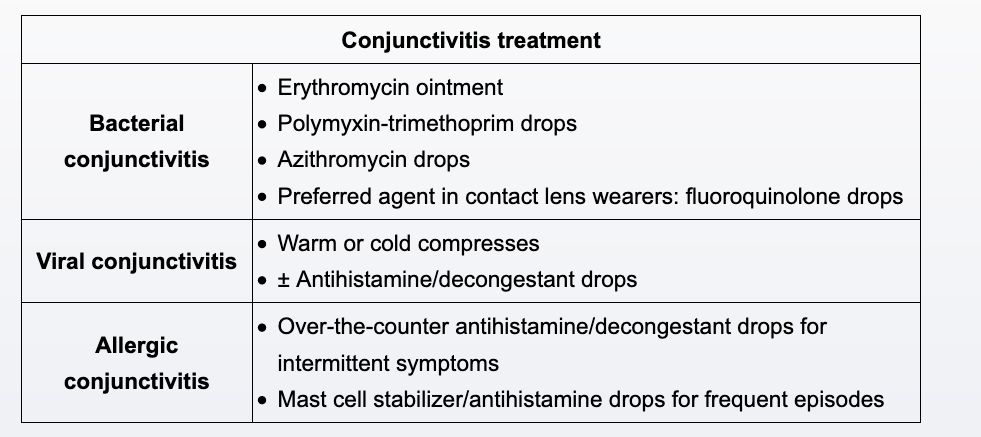
Bacterial conjunctivitis is highly contagious and presents with conjunctival erythema and mucopurulent discharge. The discharge is often thick and accumulates quickly, causing matting of the eyelid. The condition is often unilateral although it can be bilateral. Bacterial conjunctivitis is usually self-limited, but topical antibiotics are prescribed to shorten symptom duration and reduce person-to-person transmission.
The most common causes of bacterial conjunctivitis are Staphylococcus aureus, Streptococcus pneumoniae, Moraxella catarrhalis, and Haemophilus influenzae. First-line treatment is typically erythromycin ointment or polymyxin-trimethoprim drops. However, the incidence of Pseudomonas aeruginosa conjunctivitis is much higher among contact lens wearers, such as this child. Therefore, topical fluoroquinolones (eg, ciprofloxacin, ofloxacin) are preferred for contact lens wearers; erythromycin, macrolides (Choice E), and polymyxin-trimethoprim have limited activity against P aeruginosa.
The most appropriate treatment is trimethoprim–polymyxin B ophthalmic drops. This patient has acute, painless eye redness and several other signs of bacterial conjunctivitis. Studies have identified features that increase the probability of a bacterial cause of conjunctivitis, including redness of the conjunctival membrane obscuring the tarsal vessels, matting of both eyes in the morning, and purulent discharge. Inability to see redness of the eyes at 20 feet decreases the likelihood of a bacterial cause. Antibiotic treatment of bacterial conjunctivitis with topical trimethoprim–polymyxin B or erythromycin can shorten the duration of symptoms, but overall, bacterial conjunctivitis is a self-limited condition from which most patients recover within 2 weeks. Antibiotics should be enlisted when there is a higher risk for complications, such as in patients who wear contact lenses; immunocompromised patients, such as those with diabetes mellitus; and patients with copious, hyperpurulent discharge of the eye.
Ceftriaxone is used to treat gonococcal infection. Typical patients with gonococcal conjunctivitis are young men with copious purulent discharge and marked conjunctival inflammation. Periocular edema and tenderness, gaze restriction, and preauricular lymphadenopathy are common with gonococcal conjunctivitis.
Because of concerns about antimicrobial resistance and cost, topical fluoroquinolones (such as levofloxacin) are not first-line therapy for routine cases of bacterial conjunctivitis. Topical fluoroquinolones are indicated for conjunctivitis in contact lens wearers as a result of the high incidence of Pseudomonas infection.
Olopatadine ophthalmic drops are used for seasonal allergies; the mucopurulent discharge, morning matting of the eyes, and lack of itching make allergic conjunctivitis a less likely cause of this patient's symptoms.
Bacterial conjunctivitis can progress to bacterial keratitis, which most commonly occurs in patients who wear contact lenses improperly (eg, overnight use) or have decreased immunity (eg, corticosteroid use).