congenital syndromes
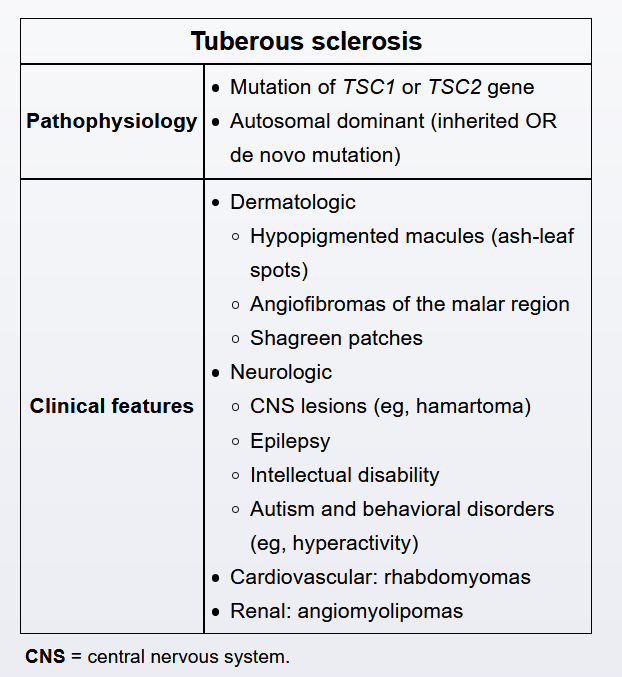

This child's seizure, hypopigmented skin lesions ("ash-leaf spots"), and mild developmental delays are concerning for tuberous sclerosis complex (TSC). TSC is caused by a mutation in 1 of 2 proteins, hamartin (TSC1 gene) or tuberin (TSC2 gene). These proteins form a complex that plays a role in cell division and differentiation. Mutations in these genes can be inherited in an autosomal dominant fashion, or they can be a de novo mutation (>80% of cases). Affected patients can develop benign tumors throughout the body, including the skin (eg, "ash-leaf spots," angiofibromas, shagreen patches), central nervous system (eg, glioneuronal hamartomas - the "tubers" of TSC), heart (eg, rhabdomyomas), and kidney (eg, angiomyolipoma).
The initial evaluation of a patient with suspected TSC should include a thorough cutaneous examination, funduscopy, and a brain MRI to evaluate for hamartomas. An electroencephalogram (EEG) is also indicated, as seizures are a predominant symptom that generally worsens over time. Seizures can be focal, general tonic-clonic, or subclinical (eg, behavioral changes). Normal EEGs serve as a baseline for future testing, while abnormal EEGs require antiepileptic therapy. Abdominal imaging to evaluate for renal lesions is recommended. If the diagnosis is uncertain, genetic testing for mutations in TSC1 and TSC2 can be performed.
The gene mutations of TSC1 or TSC2 cannot be identified on routine karyotyping nor is genetic testing indicated as part of the initial evaluation for suspected TSC.
The natural history of tuberous sclerosis complex (TSC) is progressive, and neurologic impairment is the leading cause of death in patients with TSC. Patients usually have significant developmental delays and uncontrollable seizures. Death may be due directly to tumors (mass effect from subependymal tumors) or from impairment caused by tumors (eg, status epilepticus, aspiration pneumonia). Optimal seizure control is strongly associated with prolonged life span. For these reasons, a brain MRI and electroencephalogram should be obtained when TSC is initially diagnosed.
Renal involvement (obstructive renal angiomyolipoma, renal failure) is the second most common cause of death after neurologic involvement. For this reason, abdominal imaging is part of the initial evaluation for suspected TSC.