congenital heart disease
hypoplastic heart
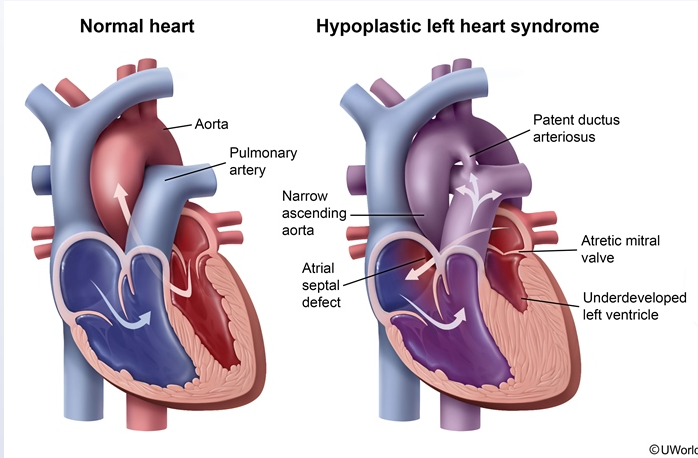
This neonate with mild cyanosis at birth followed by rapid clinical deterioration on day of life 1 most likely has hypoplastic left heart syndrome (HLHS). Patients with HLHS, a ductal-dependent congenital heart defect, have an underdeveloped left ventricle and aorta as well as an atretic mitral and/or aortic valve. The right ventricle is therefore responsible for supplying both pulmonary and systemic blood flow.
For the right side of the heart to adequately oxygenate and perfuse the body, oxygenated blood must be delivered to the right atrium (via an atrial septal defect or patent foramen ovale) and blood must flow from the pulmonary artery to the aorta via a patent ductus arteriosus (PDA). The mixing of oxygenated and deoxygenated blood in the right atrium accounts for mild cyanosis immediately after birth. As pulmonary vascular resistance physiologically decreases and the PDA closes around day of life 1, neonates with HLHS rapidly develop severe cyanosis, respiratory distress, and cardiogenic shock due to inadequate systemic perfusion. Often, no murmur is audible, but a single S2 may indicate an absent aortic valve or developing pulmonary hypertension.
Immediate administration of prostaglandin E1 in patients with suspected HLHS is required to maintain the patency of the ductus arteriosus and, in turn, systemic perfusion.
Tetralogy of Fallot and truncus arteriosus are cyanotic heart defects, but they are not ductal-dependent. Tetralogy of Fallot may present with "tet" spells, which are episodes of severe cyanosis due to right ventricular outflow obstruction. Truncus arteriosus typically presents in the neonatal period with signs of heart failure (eg, respiratory distress, poor feeding) due to excessive pulmonary blood flow. With these lesions, a systolic ejection murmur is typically heard.
A 1-day-old boy is in the newborn nursery for routine care. He was born to a 35-year-old mother at 38 weeks gestation via normal spontaneous vaginal delivery. There were no known complications with the pregnancy or delivery. The patient has breastfed several times and has voided and had a bowel movement. At 24 hours of life, standard pulse oximetry screening shows oxygen saturation of 89% in the right upper extremity and 88% in the left lower extremity. Physical examination reveals a slightly dusky-appearing infant who is crying and moving all extremities equally. Auscultation reveals a regular rate and rhythm with no murmurs. Over the next few hours, the patient develops increasing respiratory distress and hypotension. Repeat pulse oximetry demonstrates oxygen saturations <80% in all extremities. Blood pressure in all extremities is symmetric but low. The extremities are cold with diminished peripheral pulses. Which of the following is the most likely diagnosis?