Compartment syndrome
Increased edema in an enclosed compartment leads to compression of neurovascular bundles. Arterial and venous occlusion in the extremity results in anoxic muscle necrosis (rhabdomyolysis). The released myoglobin is filtered and degraded in the kidney. Heme pigment from myoglobin degradation:
- Is directly toxic to proximal tubular cells
- Combines with Tamm-Horsfall protein to form tubular casts
- Induces vasoconstriction, reducing medullary blood flow
These mechanisms lead to acute renal failure (ARF), particularly in volume-depleted states (eg, hemorrhage), which worsens vasoconstriction and cast formation.
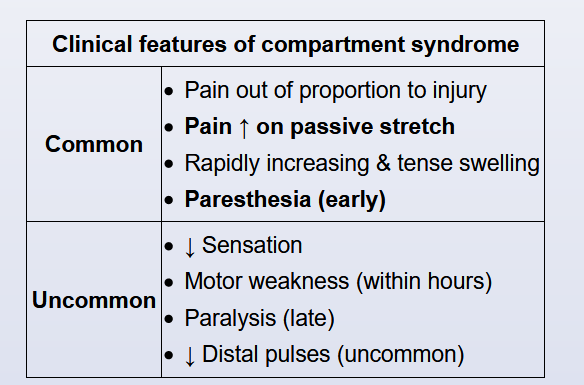
Rapidly worsening limb pain and swelling with paresthesias in a crush injury (evidenced by leg hematoma) is highly concerning for acute compartment syndrome (CS). Measurement of tissue pressures is diagnostic: Pressure >30 mm Hg or delta pressure (diastolic blood pressure − compartment pressure) <20-30 mm Hg indicates significant CS. Serial measurements should be performed even if initial pressures are within normal limits. If compartment pressures are improving, patients may be observed closely. Patients with elevated compartment pressures not improving rapidly require fasciotomy to avoid permanent loss of function from nerve and muscle injury.
Signs and symptoms of compartment syndrome (CS) are unreliable, and a high index of suspicion is needed to make the diagnosis. Disease severity cannot be assessed based on clinical features alone. Time to intervention is the most important factor predicting complete functional recovery of the limb. All constrictive coverings (casts, dressings) should be removed and supplemental oxygen given. Supportive measures to maintain perfusion pressure include keeping the limb at torso level and treating hypotension if present. Fasciotomy is the definitive treatment of choice.