cirrhosis
- related: GI
- tags: #note
Things to know for cirrhosis patients
- BM per day: lactulose or rifaximin
- Volume status: on lasix and aldactone
- Last endoscopy: any varices
- Last cancer screening: US/CT/AFP
- Transplant?
- Hx of SBP
- TIPS procedures?
Ascites? GI bleed
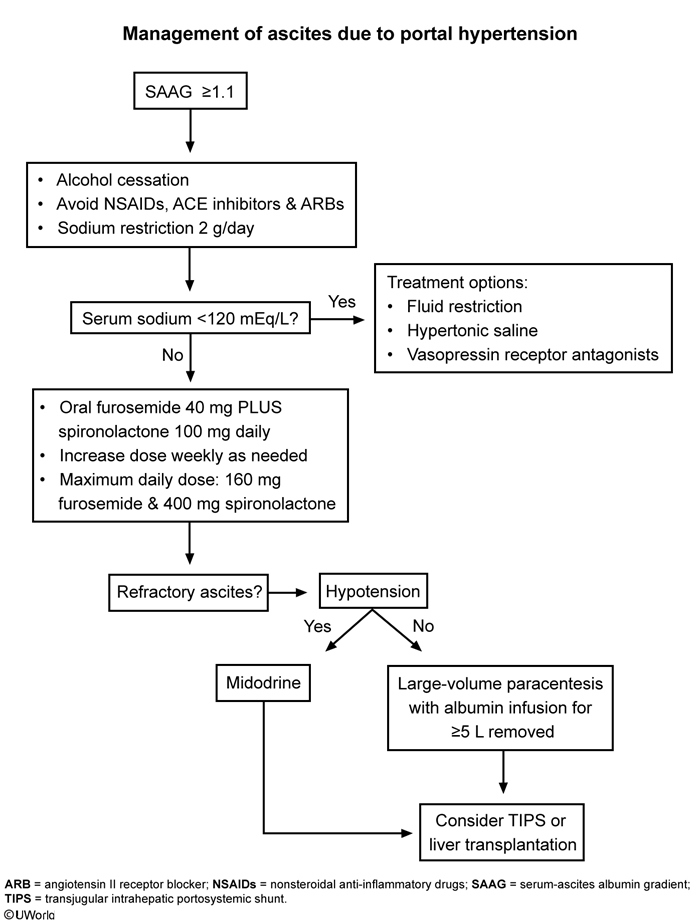
Patients without symptom improvement and serum sodium > 120 mEq/L require combination oral high-dose spironolactone and low-dose furosemide to reduce fluid retention and avoid hyperkalemia. Diuretics are titrated until symptoms improve. Spironolactone is used as a single agent in patients with profound hypokalemia. Intravenous furosemide should be avoided due to the risk of acute prerenal azotemia, which could be confused with hepatorenal syndrome. Patients with refractory ascites require large-volume paracentesis, midodrine, transjugular intrahepatic portosystemic stent-shunt (TIPS), or liver transplant depending on response.
Fluid restriction can help patients with serum sodium < 120 mEq/L. NSAIDs, angiotensin-converting enzyme inhibitors, and angiotensin II receptor blockers should be avoided in cirrhotics as they can reduce glomerular filtration rate and precipitate renal failure.
Referral for liver transplant evaluation should be considered at every visit. Referral requires patient abstinence from alcohol and drugs for about 6 months and enrollment in an alcohol rehabilitation program.
Therapeutic paracentesis is usually indicated to reduce intra-abdominal pressure in symptomatic patients (eg, shortness of breath, abdominal pain, and early satiety). It is also used to treat some patients with ascites refractory to initial diuretic therapy.
- spirnolactone: 100, lasix 40 go up to aldactone 400, lasix 160, increase every 3-5 days
EGD
This patient's presentation - newly developed ascites, serum albumin-ascites gradient (SAAG) >1.1, thrombocytopenia, elevated INR, and splenomegaly - is consistent with decompensated cirrhosis, likely due to nonalcoholic steatohepatitis. Current guidelines recommend a screening upper endoscopy (eg, esophagogastroduodenoscopy [EGD]) in patients with cirrhosis at the time of diagnosis to document the presence of varices.
Indications for prophylaxis to reduce risk of hemorrhage in patients with documented varices are based on varix size, presence of decompensated cirrhosis, and signs indicating high-bleed risk (Table). Nonselective beta blockers (eg, propanolol, nadolol) are typically first-line agents for those who require prophylaxis, with endoscopic variceal ligation (EVL) generally reserved for patients with large varices or who cannot tolerate medications. Patients who undergo EVL require repeat EGD every few weeks until varices are obliterated.
Beta blockers do not prevent the formation of varices, are not recommended in patients without varices, and should not be started prior to EGD (Choice B)