cervical myelopathy in RA
- related: Rheumatology, rheumatoid arthritis
- tags: #rheumatology
This patient’s presentation is most consistent with cervical myelopathy, likely due to atlanto-axial (C1-C2) subluxation from rheumatoid arthritis (RA). Risk factors for cervical subluxation include late-onset RA, elevated C-reactive protein, rapidly progressive peripheral joint disease, and early subluxation of peripheral joints. C1-C2 is the only spinal segment lined by a synovial membrane. Patients with RA can develop synovitis with erosions that destroy adjacent ligaments anchoring C1-C2, causing eventual subluxation of C1 relative to C2 (most often anteriorly). This creates pressure on the adjacent spinal cord and results in cervical myelopathy.
"Deep tendon reflexes are 3+ in both the upper and lower extremities bilaterally with a few beats of unsustained clonus at the ankles. Her gait is unsteady. She cannot walk heel-to-toe without assistance. Proprioception is decreased at both ankles."
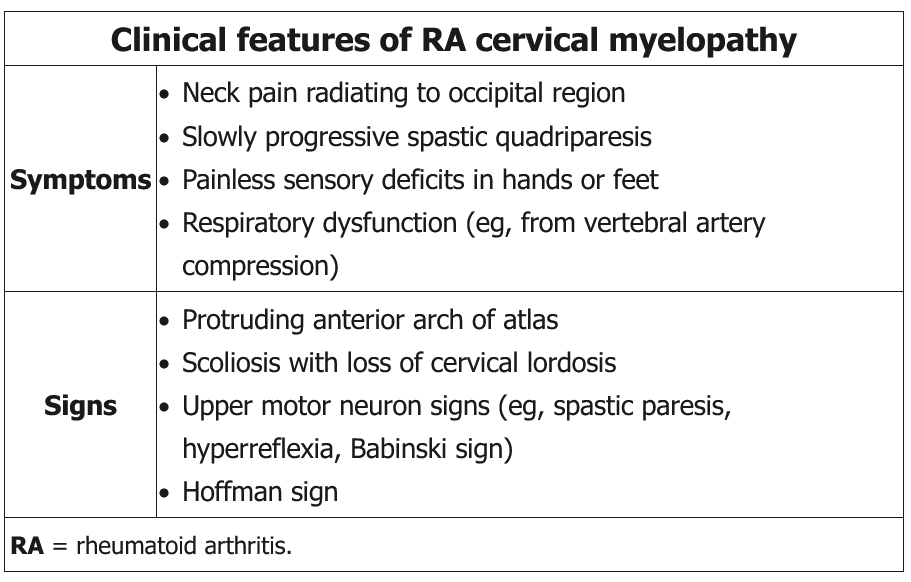
Patients present with symptoms/signs listed in the above table. Plain radiographs are sometimes difficult to interpret but may show separation between C1 and C2. A spinal MRI is preferred to visualize the cervical spine for spinal cord compression, bony erosions, and synovitis. Patients with subluxation without signs of cord compression can be treated medically with neck collars and close monitoring with fall prevention. Patients with signs of cord compression usually require surgery for spinal stabilization. This patient is very symptomatic and should undergo cervical MRI.