Catatonia
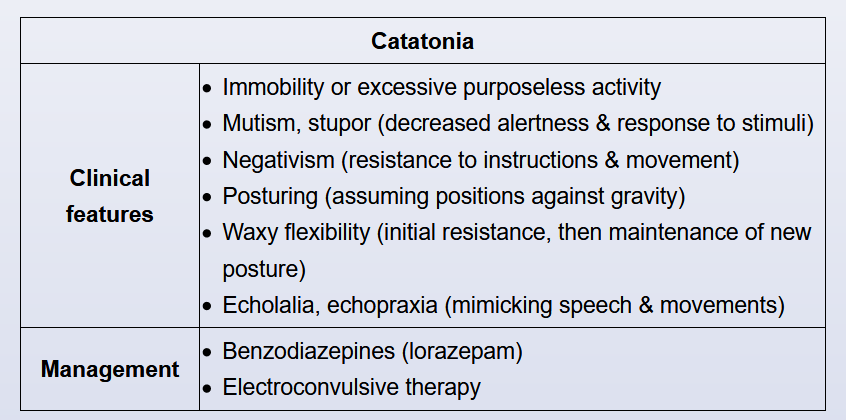
This patient's history of schizophrenia, current unresponsiveness, immobility, and catalepsy (passively allowing the examiner to position him) are all suggestive of catatonia. Catatonia is a syndrome (not a specific disorder) of marked psychomotor disturbance that occurs in severely ill patients with psychotic disorders, bipolar disorder with psychotic features, major depression with psychotic features, autism spectrum disorder, and medical conditions (infectious, metabolic, neurologic, rheumatologic). Catatonia can range from stupor to marked agitation (catatonic excitement), which contributes to difficulties in recognition. In DSM-5, a single set of criteria is used to diagnose catatonia across diagnostic categories. Characteristic features include decreased motor activity, lack of responsiveness during interview, or excessive and peculiar motor activity. In severe cases, the patient may need close supervision to avoid harm to self or others. The condition should be treated promptly, as potential risks include malnutrition, hyperpyrexia, exhaustion, and self-inflicted injury.
The treatment of choice for catatonia is benzodiazepines (especially lorazepam) and/or electroconvulsive therapy (ECT). A lorazepam challenge test (intravenous bolus of lorazepam 1-2 mg) resulting in partial, temporary relief within 5-10 minutes confirms the diagnosis of catatonia. However, a negative response does not rule out catatonia, and patients often need repeated doses. ECT is recommended in urgent clinical situations or when the patient responds poorly to benzodiazepines. Studies indicate that 60%-80% of patients recover with benzodiazepines alone or benzodiazepines followed by ECT.
Avoid antipsychotics (can worsen symptoms).