cat bite
- related: ID
- tags:
- Cat bites are more likely than dog bites to cause infection because of cats' sharp, narrow teeth
- Infections are caused by organisms from the animal's mouth flora and the host's skin flora. This flora comprises a mix of anaerobic and aerobic organisms, including streptococci, staphylococci, and Bacteroides, Fusobacterium, Porphyromonas, and Pasteurella species.
- [[Pasteurella]] is a facultative anaerobic gram-negative rod that is the most common bacteria in a cat's mouth. Pasturella multocida is found in nearly 50% of cat bites.
- Intravenous piperacillin-tazobactam, ampicillin-sulbactam, imipenem, or meropenem would address these organisms but not potential methicillin-resistant Staphylococcus aureus (MRSA). If pus is present, the patient has MRSA risk factors such as a previous MRSA infection or colonization within the last year, or local MRSA prevalence is high, then coverage should also include agents that target MRSA, such as vancomycin or daptomycin. Consequently, the combination of ampicillin-sulbactam and vancomycin (3-5 day course ampicillin-sulbactam) would be the best choice for empiric antibiotic coverage because this regimen is effective against serious infections caused by MRSA and the microbiota of a cat's mouth.
- Neither vancomycin nor clindamycin provides adequate coverage against Pasteurella species, so this regimen would not be effective for a cat bite–associated infection.
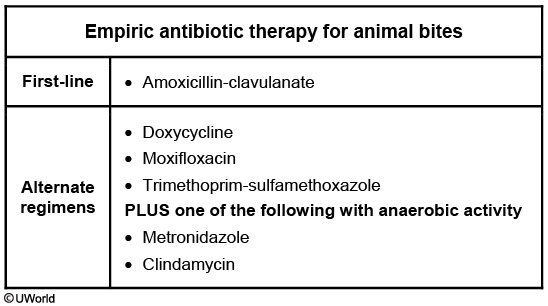
- If a patient is allergic to penicillin, a combination of trimethoprim-sulfamethoxazole, or a fluoroquinolone, or doxycycline plus clindamycin or metronidazole can be used.
- Intravenous antibiotic options include β-lactam or β-lactamase inhibitors (ampicillin-sulbactam, piperacillin-tazobactam), carbapenems (imipenem, meropenem, ertapenem), or ceftriaxone or a fluoroquinolone plus clindamycin or metronidazole.
- Ceftriaxone and metronidazole would be effective against many of the organisms encountered in a cat bite–associated skin infection, but it would not cover the possibility of MRSA infection in this patient.
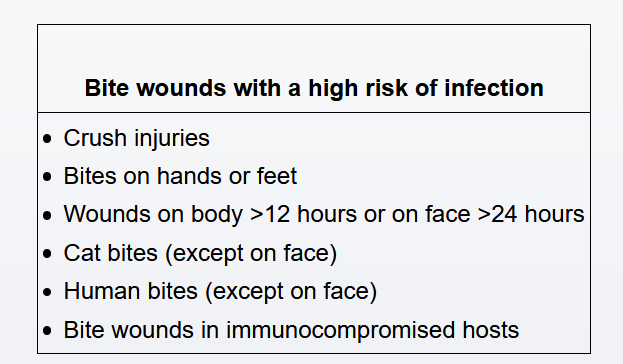
Mammalian bites can lead to infection from either oral flora of the animal (eg, Pasteurella, oral anaerobes) or skin flora of the patient (eg, Streptococcus pyogenes, Staphylococcus aureus). Cat bites are considered particularly high-risk as feline teeth are thin and sharp, resulting in puncture wounds that inoculate bacteria deep into tissue. Bites also carry a higher risk of infection if they are on the hands/feet, >12 hours old, and in immunocompromised patients.
For patients with any of these historical features, wounds should be left open to heal by secondary intention and antibiotic prophylaxis should be provided. Amoxicillin-clavulanate is the first-line agent for prophylaxis following mammalian bites as it provides coverage against both gram-negative (eg, Pasteurella) and gram-positive (eg, S pyogenes) organisms as well as oral anaerobes.
Clindamycin has activity against oral anaerobes and gram-positive organisms (eg, Streptococcus, Staphylococcus) but is not active against gram-negative organisms (eg, Pasteurella). Similarly, trimethoprim-sulfamethoxazole has activity against Pasteurella but lacks activity against oral anaerobes or Streptococcus. These agents can be used in combination for bites in penicillin-allergic patients, but neither is sufficient as monotherapy.