brain death exams
- related: ICU
- tags: #icu
Brain Death

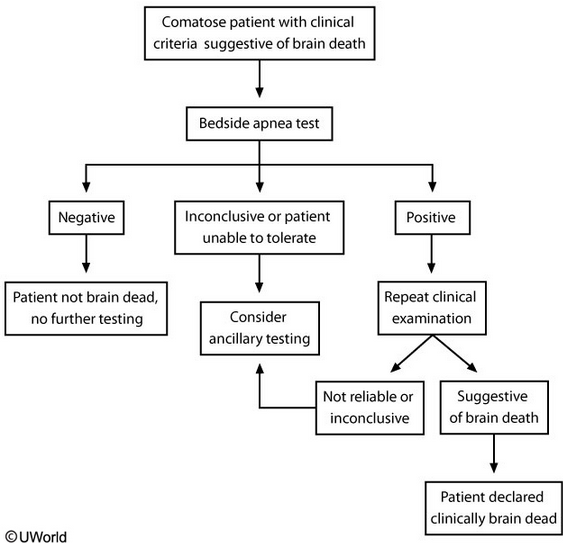
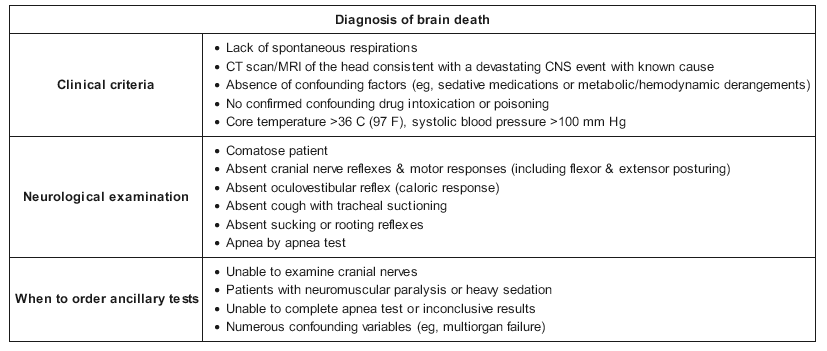
When clinical criteria suggest brain death, the best next step is apnea testing. Patients must be hemodynamically stable with a body temperature > 36 C (97 F), normal pH, and normal PaCO2/PaO2 levels. Apnea testing objectively confirms brainstem failure if the patient cannot generate spontaneous breaths or trigger the ventilator in response to elevated PaCO2 levels > 10 minutes after disabling control mode (Choice E).
Patients are first pre-oxygenated with 100% oxygen for 10 minutes using existing ventilatory support, and then mechanical ventilation is discontinued. However, they should continue to passively receive 100% oxygen while the chest and abdomen are observed for spontaneous respirations for approximately 10 minutes. If spontaneous respirations are observed, the apnea test is negative and the patient is not brain dead. A positive test is defined as no spontaneous respirations and requires another clinical brain death examination for confirmation. In addition, repeat ABG must confirm that the PaCO2 was > 60 mm Hg or that it increased > 20 mm Hg from the baseline ABG. Patients who cannot tolerate apnea testing or have inconclusive results require ancillary diagnostic tests to confirm brain death.
(Choice A) The atropine response test involves administering atropine and observing for an increase in heart rate (> 3%). Although the vagal nucleus in the medulla may be one of the last functions lost in brain death, the atropine response test provides a limited assessment and has not been well validated for confirming brain death.
(Choice C) Cerebral blood flow testing (e.g., cerebral angiogram or cerebral scintigraphy) is the gold standard test for brain death confirmation, but it is highly invasive and not used routinely as the initial step for diagnosing brain death. Cerebral blood flow testing may be used in patients with an unreliable clinical examination or bedside apnea test.
(Choice D) Current guidelines do not recommend EEG with ECI protocol for brain death confirmation, as it is susceptible to excessive artifact from other electrical devices in the ICU that make it less reliable. In addition, EEG is very sensitive to the effects of sedative medications and metabolic derangements, and therefore can be easily confounded by those variables.