Ankylosing Spondylitis
- related: Rheumatology
- tags: #rheumatology
Demographics
Ankylosing spondylitis is a chronic inflammatory disease affecting the axial skeleton, entheses, and peripheral joints. In contrast to other forms of spondyloarthritis, sacroiliac joint involvement is considered an essential feature of ankylosing spondylitis. Ankylosing spondylitis has a strong familial predilection and the strongest association with HLA-B27 among the forms of spondyloarthritis, being present in up to 95% of patients. Although a male predominance of 2-3:1 has been described, women usually have milder and underappreciated disease; prevalence may actually be similar between genders. Disease can begin as early as adolescence, but peak age of diagnosis is between 20 and 30 years.
Symptoms
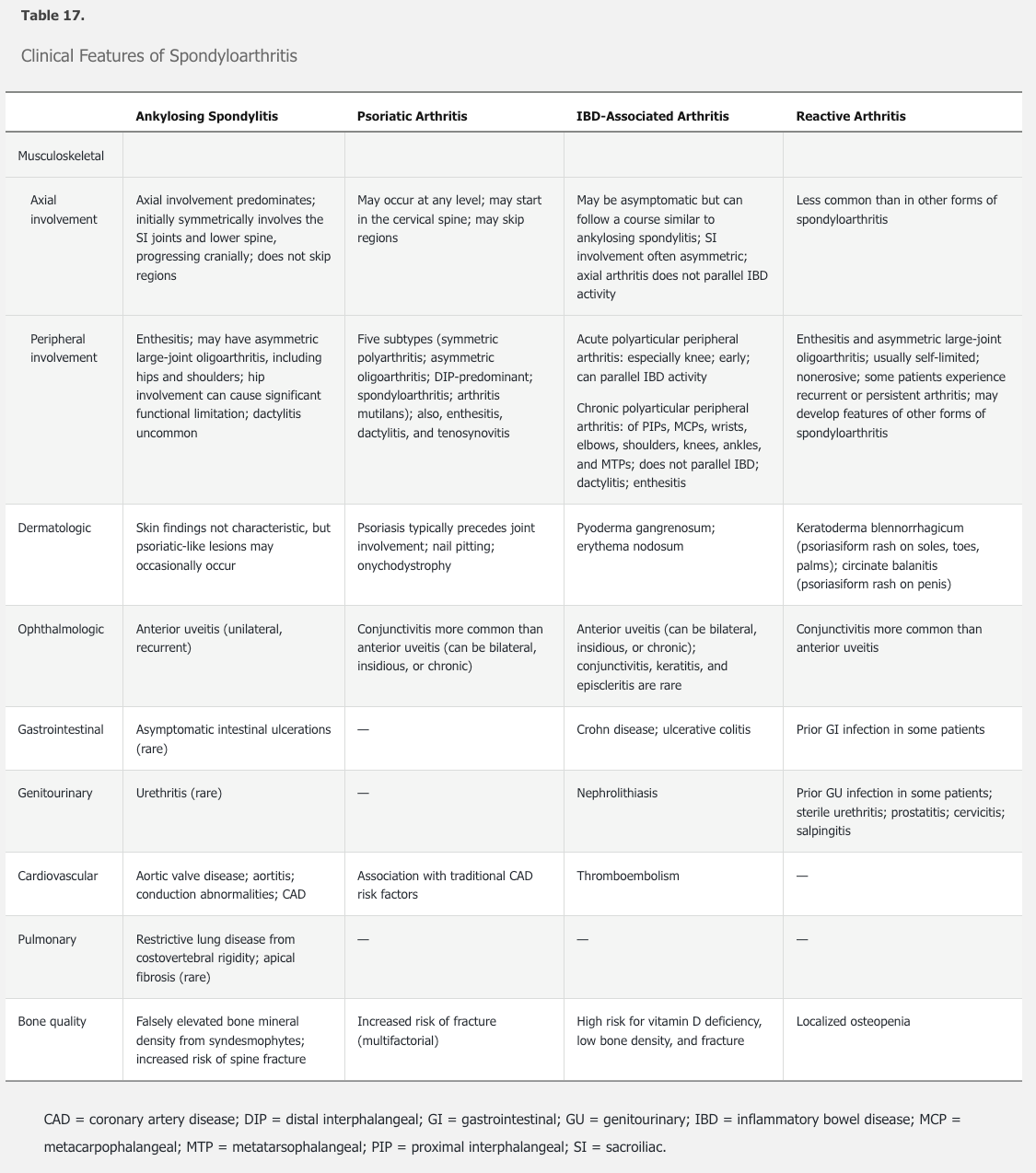
Symptoms of inflammatory back pain are most frequently the presenting complaint. Spinal involvement begins in the lumbar region and tends to ascend. Buttock pain may indicate sacroiliac joint involvement, which is characteristically bilateral. About one third of patients develop hip joint involvement and about one third develop peripheral arthritis elsewhere, often in the shoulders. Enthesitis most often manifests as Achilles tendinitis. Dactylitis occurs in fewer than 10% of patients.
Physical examination, particularly in more advanced disease, can be highly characteristic. With active inflammation, tenderness over the sacroiliac joints is often the first sign of disease. Over time, marked reduction in spinal mobility can occur in all planes, and chest expansion becomes reduced. Flexion deformity at the neck and thoracic hyperkyphosis may lead to a hunched posture. A loss of lumbar lordosis and restricted range of motion in the hips may also be evident.
- Low back pain (onset age <40, insidious onset, better with exercise, no improvement with rest, pain at night)
- Hip & buttock pain
- Enthesitis (inflammation at the site of insertion of a tendon to the bone)
- Systemic symptoms (eg, fever, chills, fatigue, weight loss)
- Acute anterior uveitis (unilateral pain, photophobia, blurry vision)
Limited chest wall expansion
Limited chest wall expansion is due to costovertebral rigidity. Normal chest wall expansion is > 5 cm after maximum forced expiration followed by maximum inspiration. Expansion < 2.5 cm is considered abnormal and suggests AS. Patients with kyphoscoliosis and deformity above T10 are at increased risk for nocturnal hypoventilation and apneic events as well as respiratory failure. Advanced AS may have x-ray findings of continuous fusion of the lumbar spine ("bamboo spine"). Treatment of respiratory impairment includes pulmonary rehabilitation and noninvasive positive-pressure ventilation.
Extra-articular Symptoms
Extra-articular manifestations of ankylosing spondylitis are not uncommon (see Table 17). Cardiac and pulmonary manifestations, including aortic valve disease, cardiac conduction abnormalities, and restrictive lung disease, are more common in ankylosing spondylitis than other forms of spondyloarthritis. In addition, vertebral compression fractures may occur with little to no trauma as the disease progresses. The cervical spine is the most common site for fractures and can be associated with neurologic complications.
Diagnosis criteria
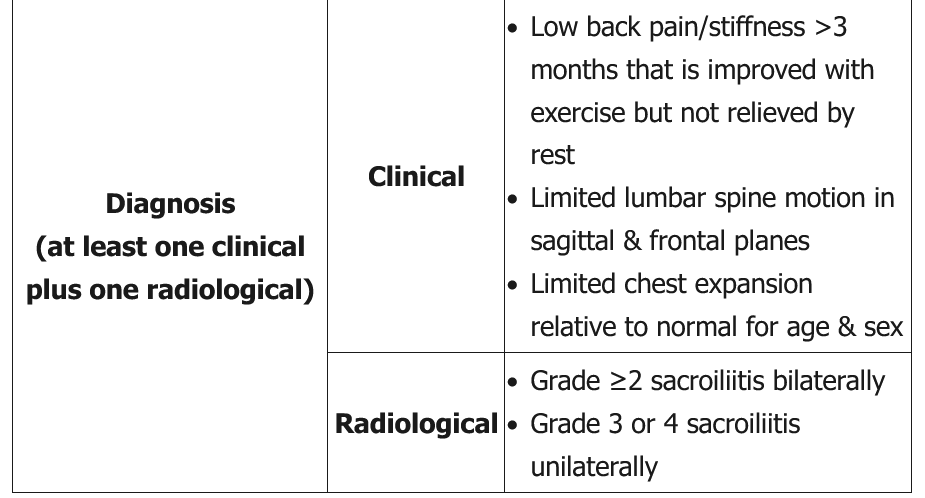
Different criteria have been proposed for the diagnosis of ankylosing spondylitis. Common requirements include the presence of inflammatory back pain for 3 or more months in a person younger than age 45 years, limited lumbar spine motion, elevated inflammatory markers, and evidence of bilateral sacroiliitis on imaging.
The presence of HLA-B27 antigen is not a diagnostic criterion for ankylosing spondylitis. However, such testing may be particularly helpful in patients with inflammatory back pain and other manifestations of ankylosing spondylitis but without evidence of sacroiliitis on imaging.
Imaging
A single anteroposterior pelvis plain radiograph to view the sacroiliac joints is an appropriate first diagnostic step in this setting, which may reveal joint space widening (early) or narrowing (late), erosions, sclerosis, and ankylosis, and can establish the diagnosis of ankylosing spondylitis. However, plain radiographs may be normal early in the course of disease, as seen in this patient. MRI of the sacroiliac joints can then be utilized, which is more sensitive for detecting early spine and sacroiliac joint inflammation. The finding of bone marrow edema on STIR or T2-weighted images with fat suppression is not specific for ankylosing spondylitis but does suggest active inflammation, particularly if found in characteristic periarticular and subchondral locations. MRI can also identify soft-tissue evidence of inflammation in the entheses, bursae, and tendons, as well as subtle structural abnormalities.
 Advanced AS may have x-ray findings of continuous fusion of the lumbar spine ("bamboo spine").
Advanced AS may have x-ray findings of continuous fusion of the lumbar spine ("bamboo spine").
CT of the lumbar spine can be useful in the diagnosis of ankylosing spondylitis when radiography of the sacroiliac joints is normal. However, it is not routinely used in the evaluation of patients for arthritis due to the high dose of radiation required.
The course of ankylosing spondylitis is variable; progression may occur over many years. Markers of a poorer prognosis include a longer duration of disease, the presence of hip joint involvement, elevation of inflammatory markers, and the presence of radiographic changes in the spine. Mortality is increased in men and correlates with disease activity.
Notes
- pt:
- sx: back pain
- morning stiffness
- improved with exercise
- insidious onset
- reduced forward flexion range, reduced chest expansion
- dx:
- xray sacroiliac joint: must have sacroiliitis
- bamboo spine
- erosions of iliac crest and ischial tuberosity
- MRI/CT if xray negative and strong suspicion
- HLA-B27 highly specific but not sensitive (negative make diagnosis unlikely)
- ANA, RF usually negative
- associations:
- restrictive lung disease, apical pulmonary fibrosis
- anterior uveitis, AR, MVP